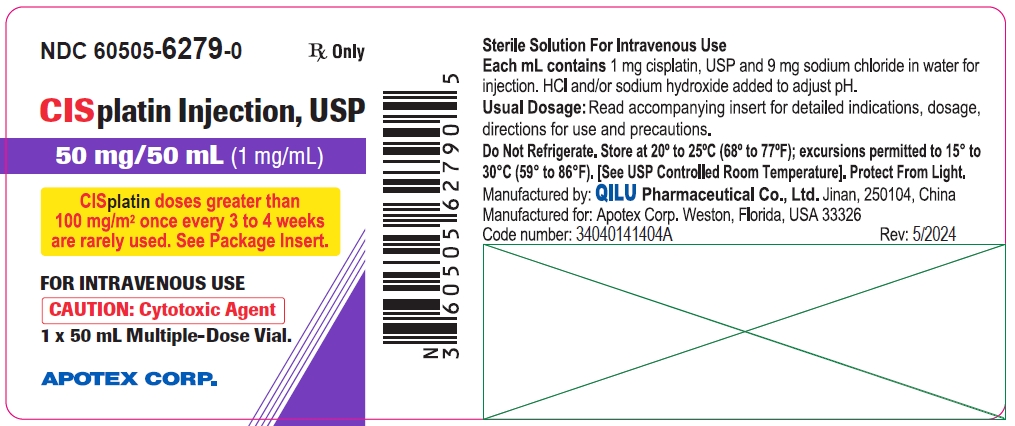
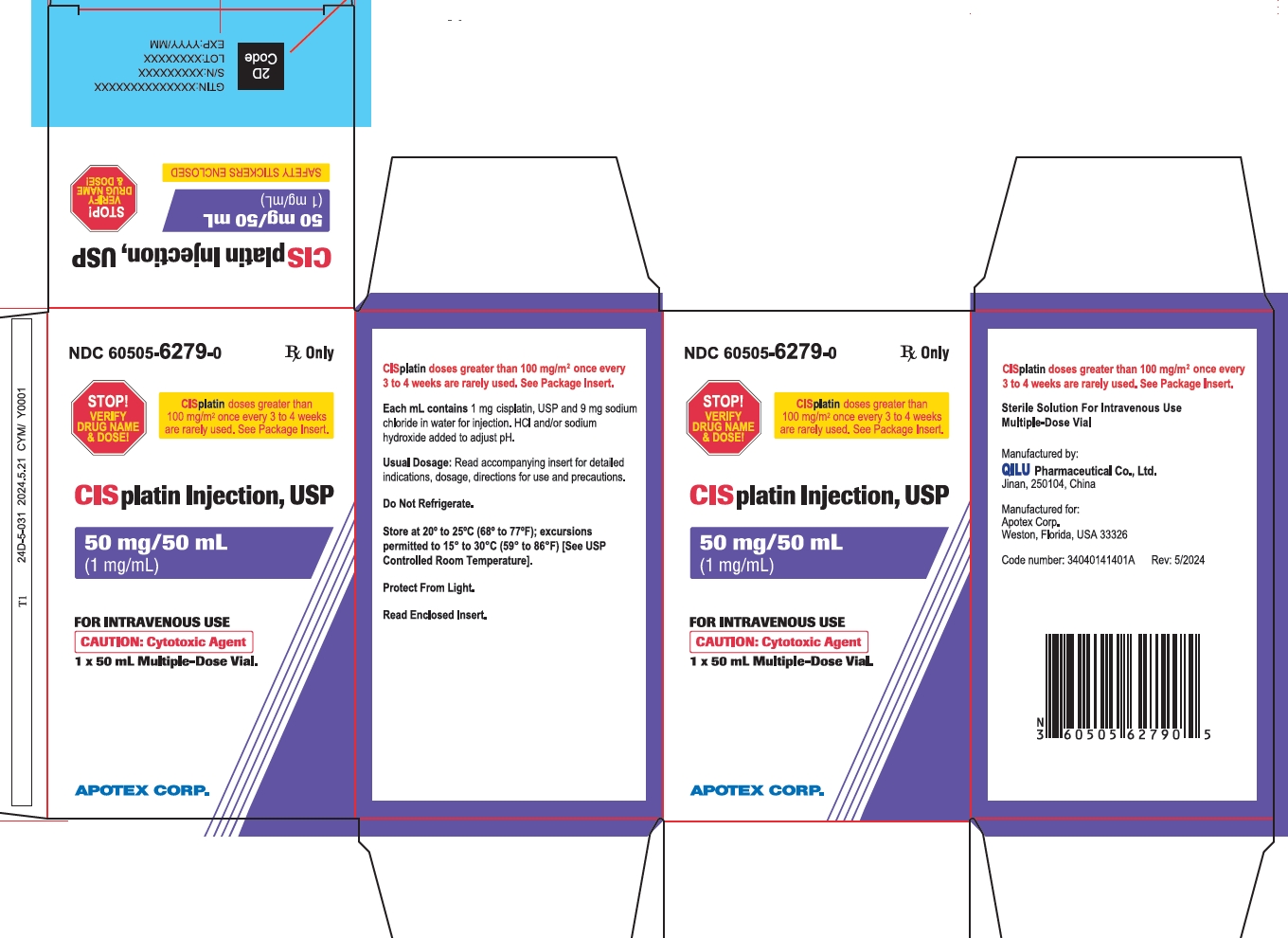
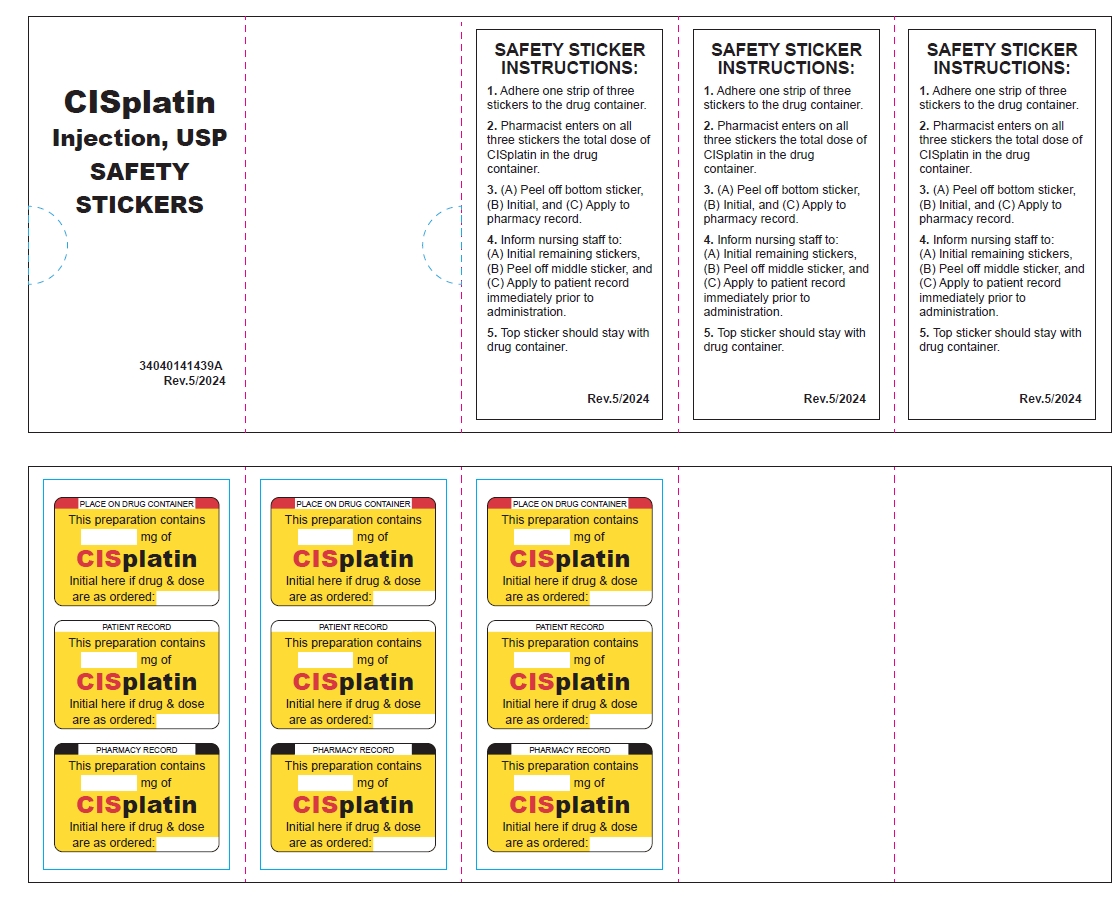
Cisplatin produces cumulative nephrotoxicity which is potentiated by aminoglycoside antibiotics. The serum creatinine, blood urea nitrogen (BUN), creatinine clearance, and magnesium, sodium, potassium, and calcium levels should be measured prior to initiating therapy, and prior to each subsequent course. At the recommended dosage, cisplatin should not be given more frequently than once every 3 to 4 weeks (see
There are reports of severe neuropathies in patients in whom regimens are employed using higher doses of cisplatin or greater dose frequencies than those recommended. These neuropathies may be irreversible and are seen as paresthesias in a stocking-glove distribution, areflexia, and loss of proprioception and vibratory sensation. Elderly patients may be more susceptible to peripheral neuropathy (see
Loss of motor function has also been reported.
Anaphylactic-like reactions to cisplatin have been reported. These reactions have occurred within minutes of administration to patients with prior exposure to cisplatin, and have been alleviated by administration of epinephrine, corticosteroids, and antihistamines.
Cisplatin can commonly cause ototoxicity which is cumulative and may be severe. Audiometric testing should be performed prior to initiating therapy and prior to each subsequent dose of drug (see
All pediatric patients receiving cisplatin should have audiometric testing at baseline, prior to each subsequent dose, of drug and for several years post therapy.
Cisplatin can cause fetal harm when administered to a pregnant woman. Cisplatin is mutagenic in bacteria and produces chromosome aberrations in animal cells in tissue culture. In mice cisplatin is teratogenic and embryotoxic. If this drug is used during pregnancy or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus. Patients should be advised to avoid becoming pregnant.
The carcinogenic effect of cisplatin was studied in BD IX rats. Cisplatin was administered intraperitoneally (i.p.) to 50 BD IX rats for 3 weeks, 3 X 1 mg/kg body weight per week. Four hundred and fifty-five days after the first application, 33 animals died, 13 of them related to malignancies: 12 leukemias and 1 renal fibrosarcoma.
The development of acute leukemia coincident with the use of cisplatin has been reported. In these reports, cisplatin was generally given in combination with other leukemogenic agents.
Injection site reactions may occur during the administration of cisplatin (see