Cortrosyn
What is Cortrosyn (Cosyntropin)?
Related Clinical Trials
Summary: Vasoplegic syndrome after cardiac surgery is common and is associated with increased morbidity and mortality. It is characterized by early and prolonged arterial hypotension, with preserved cardiac output and low systemic vascular resistance. Vasoplegic syndrome therefore shares pathophysiological features with septic shock. There are no data in the literature on the function of the hypothalamic-p...
Summary: This study will evaluate the feasibility of using a sub-therapeutic dose of a fluorine-18 analogue of NP-59 (\[18F\]FNP-59) to image the adrenal gland. Some participants are healthy normal subjects but have undergone interventions to manipulate hormones while other participants have known adrenal pathology.
Summary: The aim of this protocol is to assess the presence and severity of primary aldosteronism pathophysiology in patients with type 2 diabetes who have, or are at-risk for developing, chronic kidney disease.
Related Latest Advances
Brand Information
See full prescribing information for CORTROSYN®.
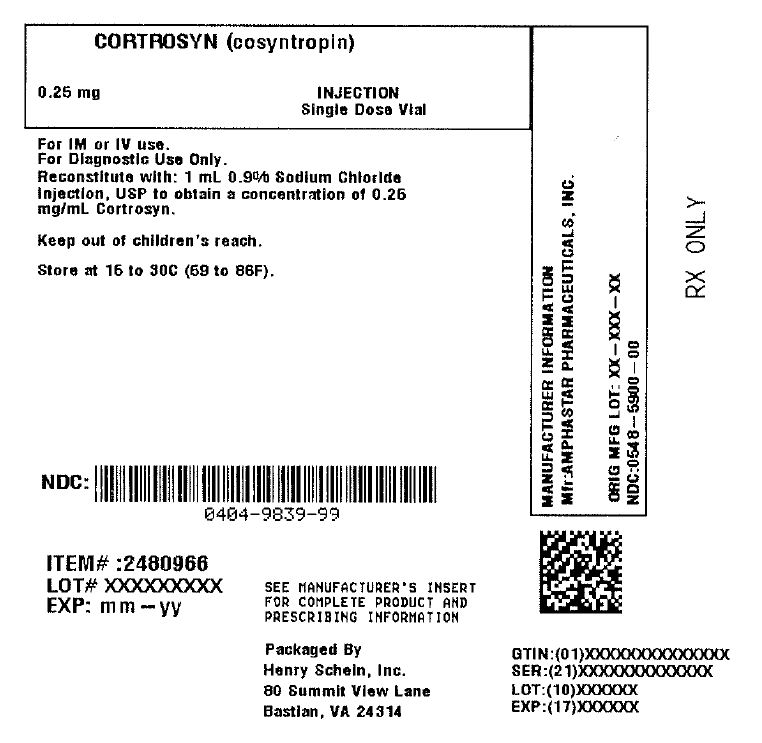
CORTROSYN (cosyntropin) for injection, for intravenous or intramuscular use
Initial U.S. Approval: 2008
- In general, stop glucocorticoids and spironolactone on the day of CORTROSYN testing. However, long-acting glucocorticoids may need to be stopped for a longer period before CORTROSYN testing
- Stop estrogen-containing drugs four to six weeks before CORTROSYN testing [see Warnings and Precautions (5.2), Drug Interactions (7)].
- The recommended dose of CORTROSYN in adults is 0.25 mg to be administered by intravenous or intramuscular injection.
- The recommended dose of CORTROSYN in pediatric patients, aged birth to 17 years, to be administered by intravenous or intramuscular injection is presented in Table 1.

- Aseptically reconstitute the lyophilized powder in the vial using 1 mL of 0.9% Sodium Chloride Injection, USP and gently swirl.
- After reconstitution, the final concentration of CORTROSYN reconstituted solution is 0.25 mg/mL.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. The reconstituted CORTROSYN solution should be clear and colorless, and free of particulates. If CORTROSYN solution is cloudy or contains particulates, do not administer.
- If the CORTROSYN reconstituted solution is not used immediately, discard the unused CORTROSYN reconstituted solution.
- anaphylactic reaction
- bradycardia
- tachycardia
- hypertension
- peripheral edema
- rash
- Accuracy of the test results can be affected by concomitant medications. Plasma cortisol levels and subsequent diagnosis of adrenocortical insufficiency following CORTROSYN administration may be inaccurate if patients are on certain medications because of their effect on cortisol or cortisol binding globulin levels
- Glucocorticoids and spironolactone: May falsely elevate plasma cortisol levels. Stop these drugs on the day of CORTROSYN testing. Long-acting glucocorticoids may need to be stopped for a longer period before CORTROSYN testing.
- Estrogen: May elevate plasma total cortisol levels. Stop estrogen containing drugs 4 to 6 weeks before CORTROSYN testing to allow cortisol binding globulin levels to return to levels within the reference range. Alternatively, concomitant measurement of cortisol binding globulin at the time of testing can be done; if cortisol binding globulin levels are elevated, plasma total cortisol levels are considered inaccurate.
Risk Summary
Available data from case reports over decades of use with cosyntropin during pregnancy have not identified an increased risk of major birth defects, miscarriage or adverse maternal or fetal outcomes. Unidentified adrenal insufficiency can result in adverse maternal or fetal outcomes (see Clinical Considerations).
Disease-associated maternal and/or embryo/fetal risk Unidentified adrenal insufficiency during pregnancy can result in maternal and/or fetal death; therefore, the diagnosis of suspected adrenal insufficiency during pregnancy should not be delayed.
Risk Summary
There are no data on the presence of cosyntropin in human milk, the effects on the breastfed infant, or the effects on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for CORTROSYN and any potential adverse effects on the breastfed infant from CORTROSYN or from the underlying maternal condition.
CORTROSYN is approved for use in pediatric patients [see Dosage and Administration (2.3)].

Cosyntropin exhibits the full corticosteroidogenic activity of natural ACTH. Various studies have shown that the biologic activity of ACTH resides in the N-terminal portion of the molecule and that the 1-20 amino acid residue is the minimal sequence retaining full activity. Partial or complete loss of activity is noted with progressive shortening of the chain beyond 20 amino acid residues. For example, the decrement from 20 to 19 results in a 70% loss of potency.
Animal, human and synthetic ACTH (1-39) which all contain 39 amino acids exhibit similar immunologic activity. This activity resides in the C-terminal portion of the molecule and the 22-39 amino acid residues exhibit the greatest degree of antigenicity. In contrast, synthetic polypeptides containing 1-19 or fewer amino acids have no detectable immunologic activity. Those containing 1-26, 1-24 or 1-23 amino acids have very little immunologic although full biologic activity. This property of CORTROSYN assumes added importance in view of the known antigenicity of natural ACTH.
Long-term carcinogenicity studies in animals to evaluate the carcinogenic potential of cosyntropin have not been conducted. Studies to evaluate mutagenic potential or impairment of fertility in animals have not been conducted.
CORTROSYN (cosyntropin) for injection 0.25 mg, in a single-dose vial for reconstitution.
Store at 20º to 25ºC (68º to 77ºF); excursions permitted between 15° to 30°C (59° to 86°F) [see USP Controlled Room Temperature].
Inform patients and/or caregivers of the early signs of hypersensitivity reactions including rash, hives, itching, facial swelling, tightness of the chest, and wheezing [see Contraindications (4), Warnings and Precautions (5.1)].
Advise patients and/or caregivers to stop taking glucocorticoids and spironolactone on the day of CORTROSYN testing. However, for patients taking long-acting glucocorticoids, advise them to stop for longer periods before CORTROSYN testing. Advise patients to stop taking estrogen-containing drugs four to six weeks before CORTROSYN testing [see Dosage and Administration (2.1), Warnings and Precautions (5.2), and Drug Interactions (7)].