Brand Name
Mepsevii
Generic Name
Vestronidase
View Brand Information FDA approval date: November 15, 2017
Classification: Lysosomal beta Glucuronidase
Form: Injection
What is Mepsevii (Vestronidase)?
MEPSEVII is indicated in pediatric and adult patients for the treatment of Mucopolysaccharidosis VII . Limitations of Use The effect of MEPSEVII on the central nervous system manifestations of MPS VII has not been determined. MEPSEVII is a recombinant human lysosomal beta glucuronidase indicated in pediatric and adult patients for the treatment of Mucopolysaccharidosis VII . Limitations of Use The effect of MEPSEVII on the central nervous system manifestations of MPS VII has not been determined.
Approved To Treat
Top Global Experts
Save this treatment for later
Not sure about your diagnosis?
Tired of the same old research?
Related Clinical Trials
Mucopolysaccharidosis VII Disease Monitoring Program (MPS VII DMP)
Summary: The objectives of this study are to characterize MPS VII disease presentation and progression and assess long-term effectiveness and safety, including hypersensitivity reactions and immunogenicity of vestronidase alfa.
Related Latest Advances
Brand Information
MEPSEVII (vestronidase alfa)
WARNING: ANAPHYLAXIS
- Anaphylaxis has occurred with MEPSEVII administration, as early as the first dose [see Warnings and Precautions (5.1)], therefore appropriate medical support should be readily available when MEPSEVII is administered.
- Closely observe patients during and for 60 minutes after MEPSEVII infusion [see Dosage and Administration (2.2), Warnings and Precautions (5.1)].
- Immediately discontinue the MEPSEVII infusion if the patient experiences anaphylaxis [see Dosage and Administration (2.2), Warnings and Precautions (5.1)].
1INDICATIONS AND USAGE
MEPSEVII is indicated in pediatric and adult patients for the treatment of Mucopolysaccharidosis VII (MPS VII, Sly syndrome).
Limitations of Use
The effect of MEPSEVII on the central nervous system manifestations of MPS VII has not been determined.
2DOSAGE FORMS AND STRENGTHS
Injection: 10 mg/5 mL (2 mg/mL) as a colorless to slightly yellow liquid in a single-dose vial.
3CONTRAINDICATIONS
None.
4ADVERSE REACTIONS
The following serious adverse reactions are described below and elsewhere in the labeling:
- Anaphylaxis
4.1Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The MEPSEVII clinical program included 23 patients aged 5 months to 25 years who received treatment with MEPSEVII at doses up to 4 mg/kg once every two weeks for up to 187 weeks. Nineteen patients were younger than 18 years of age.
Table 2 summarizes the adverse reactions that occurred in Study 301, a randomized start trial in 12 patients with MPS VII between the ages of 8 and 25 years
Adverse reactions in Table 2 occurred in one or more patients treated with MEPSEVII at a dosage of 4 mg/kg at a higher patient frequency than placebo. Adverse reaction incidence rates are presented in the table below to account for the different duration of exposure to active treatment vs. placebo.
n = number of reactions
*Adverse reaction incidence rates calculated per 8.3 patient years for exposure to MEPSEVII, and 2.7 years of exposure for placebo
Febrile Convulsion
One patient receiving a dose of 4 mg/kg experienced a febrile convulsion during MEPSEVII treatment at Week 66. The infusion was stopped, the patient received anticonvulsants, antipyretics and antibiotics, and the adverse reaction resolved. The patient subsequently was re-challenged without recurrence and continued on treatment.
4.2Immunogenicity
As with all therapeutic proteins, there is potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies in the studies described below with the incidence of antibodies in other studies to other vestronidase alfa products may be misleading.
Immunogenicity data were available from 23 patients who received MEPSEVII for up to 187 weeks of treatment. Eighteen out of 23 (78%) patients developed anti-vestronidase alfa-vjbk antibodies (ADA). Ten of the 18 (55.6%) ADA-positive patients were tested positive for neutralizing antibodies (NAb). There is no correlation between ADA titer and NAb development.
Six treatment-naïve patients had pre-existing ADA titers at baseline. ADAs were detected in five of these six patients post-treatment. The post-treatment ADA titers were the same as or below the baseline ADA titer values in two patients, but one of these two patients was positive for NAb. ADA titer values after treatment increased 64-fold, 128-fold, and 364-fold, respectively, in the other three patients.
The presence of ADA titer did not appear to affect reduction in urinary glycosaminoglycans (uGAGs).
5DESCRIPTION
Vestronidase alfa-vjbk is a recombinant human lysosomal beta glucuronidase which is a purified human enzyme produced by recombinant DNA technology in a Chinese hamster ovary cell line.
Purified vestronidase alfa-vjbk exists as a homotetramer, with each monomer consisting of 629 amino acids. The calculated isotope average molecular mass of each non-glycosylated peptide chain is 72,562 Da.
The amino acid sequence for vestronidase alfa-vjbk is the same as the amino acid sequence for human beta-glucuronidase (GUS).
MEPSEVII (vestronidase alfa-vjbk) injection for intravenous infusion is a sterile, preservative-free, non-pyrogenic, colorless to slightly yellow liquid supplied in a single-dose vial. Each mL of solution contains vestronidase alfa-vjbk (2 mg), L-histidine (3.1 mg), polysorbate 20 (0.1 mg), sodium chloride (7.88 mg) and sodium phosphate monobasic dihydrate (3.12 mg). The pH of the solution is 6.0.
6CLINICAL STUDIES
The clinical program for MEPSEVII included 23 patients with MPS VII, 17 of whom were evaluable for efficacy, 20 for safety, and 23 for immunogenicity. Patients were enrolled in clinical trials and expanded access protocols receiving treatment at doses up to 4 mg/kg once every two weeks for up to 187 weeks. The patients ranged in age from 5 months to 25 years. Sixteen patients were younger than 18 years of age.
Studies301 and 202
Study UX003-CL301 (referred to as Study 301, NCT02230566) was a randomized start trial of MEPSEVII 4 mg/kg every two weeks in patients with MPS VII. Twelve patients were randomized to one of four placebo durations before crossing over to active treatment. Three patients received MEPSEVII immediately for a duration of 48 weeks, 3 patients received placebo for 8 weeks then MEPSEVII for 40 weeks, 3 patients received placebo for 16 weeks then MEPSEVII for 32 weeks, and 3 patients received placebo for 24 weeks then MEPSEVII for 24 weeks. Of the 12 patients enrolled in the trial, 4 were male and 8 were female and ranged in age from 8 to 25 years (median 14 years). Nine patients were younger than 18 years of age. The majority of the patients were white (75%), with 50% of Hispanic or Latino ethnicity. Patients who were enrolled in Study 301 were eligible to roll over to Study UX003-CL202 (referred to as Study 202, NCT02432144), an open-label extension trial in which patients received additional doses of MEPSEVII at 4 mg/kg intravenously every other week for up to 144 weeks. Ten patients rolled over directly from the end of Study to Week 0 of Study 202, while 2 patients (17%) had treatment gaps before enrolling in Study 202.
In Study 301, motor function, forced vital capacity, and visual acuity were assessed after 24 weeks of MEPSEVII treatment and measured against pre-specified minimal important differences. The extremely small population of patients with MPS VII globally necessitated the enrollment of all patients able to participate resulting in a highly heterogeneous group. Clinical endpoints were not assessable in some patients due to their extent of disease, age or level of cognition. Repeated assessments of the six minute walk test (6MWT) were feasible in ten of 12 patients and are described further below. Of the three patients who improved on their 6MWT (Figure 1, left panel), two also were noted to have improvement in balance and gross motor proficiency as assessed by the Bruininks-Oseretsky Test of Motor Proficiency (BOT-2).
In this trial, the mean difference in 6MWT distance between MEPSEVII and placebo treatment periods in patients able to perform the test at baseline and subsequent visits through Week 24 is shown in Table 3. The mean difference in 6MWT distance increases with increased treatment duration, however, due to the small size of the trial, standard errors are large.
*ANCOVA analysis of change from baseline in least squares (LS) mean between placebo and MEPSEVII for different periods, after adjusting for study cohort, age, and baseline 6MWT distance. Patients who used assistive devices were imputed as zeros in the analysis.
**Number and treatment assignment of patients included in the analysis was based upon a randomized start trial design and patient ability to complete testing. Due to no placebo period for the three patients who received 48 weeks of MEPSEVII in the first cohort of the randomized start design, more data were available for analyses during the treatment period (n=8) than during the placebo period (n=5). While data from 8 participants were available at each time point, due to missing observations, the 8 participants were not the same across all time points.
The observed individual 6MWT distances for the 10 patients who could perform the test in Study 301 and Study 202 through Week 184 are presented in Figure 1. The course of three patients with improvement in distance walked of at least 60 meters during the 301 Study compared to the start of MEPSEVII treatment (Week 0) is shown in the left panel; the relatively stable course in the remaining seven patients, including those who used assistive devices, is shown in the right panel.
Figure 1. 6MWT Distance for MPS VII Patients in Studies 301 and 202
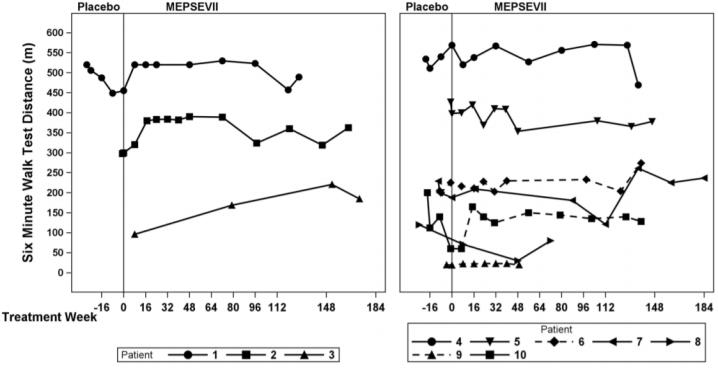
Patient 10 did not use an assistive device at baseline but started using an assistive device post-baseline from Treatment Week 8. Patients 6 and 9 consistently used an assistive device at all visits. A solid line indicates the unassisted assessments and a dotted line indicates the assisted assessments.
Liver and Spleen Volume
In Study 301, imaging by MRI or ultrasound to assess liver and spleen volume was performed in seven of the 12 patients. Most liver volumes were normal or below normal size at baseline (mean 1,591 mL, range 742 to 2,207 mL), and on average were unchanged after treatment (mean 1,459 mL, range 876 to 1,851 mL).
Spleen volumes generally were normal or below normal size at baseline (mean 325 mL, range 131 to 491 mL) and on average were unchanged after treatment (mean 360 mL, range 200 to 582 mL).
Study 203
UX003-CL203 (referred to as Study 203; NCT 02418455 ) was an open-label, uncontrolled single arm study that enrolled 8 patients less than 5 years of age who received MEPSEVII at a dose of 4 mg/kg every two weeks for 48 weeks of treatment and up to an additional 240 weeks during an optional continuation period. The study evaluated urinary GAG excretion, growth and hepatosplenomegaly. With long-term treatment, urinary GAG levels remained decreased upon exposure to MEPSEVII. At baseline, all 8 patients had impaired growth, and height remained near the 5th percentile relative to age-matched gender norms throughout the trial. No significant changes in hepatosplenomegaly were observed.
Other Investigations
Study UX003-CL201 (referred to as Study 201, NCT01856218) was a single arm, open-label, dose exploration trial completed outside the United States that enrolled three MPS VII patients, ranging in age from 5 years to 25 years. Two patients were male; two patients were white and one was Asian. After 120 weeks of exposure to MEPSEVII, one patient demonstrated a 21% improvement over baseline in forced vital capacity (FVC% predicted) on pulmonary function testing in addition to a 105 meter improvement in the 6MWT. Two other patients with baseline hepatosplenomegaly had reduction in liver volume (24% and 53%) and spleen volume (28% and 47%) after 36 weeks of MEPSEVII treatment.
Expanded access to MEPSEVII treatment was provided to a pediatric patient with MPS VII who required continuous ventilatory support at the start of treatment and was subsequently able to tolerate 9 hours daily off ventilator support after 164 weeks of MEPSEVII treatment.
7HOW SUPPLIED/STORAGE AND HANDLING
MEPSEVII (vestronidase alfa-vjbk) injection is a colorless to slightly yellow liquid supplied as a carton containing one 10 mg/5 mL (2 mg/mL) single-dose vial (NDC 69794-001-01).
Store under refrigeration at 2°C to 8°C (36°F to 46°F). Do not freeze or shake. Protect from light.
8PATIENT COUNSELING INFORMATION
Anaphylaxis
Advise patients and caregivers that anaphylaxis has occurred with MEPSEVII administration. Inform patients of the signs and symptoms of anaphylaxis, and have them seek immediate medical care should signs and symptoms occur
Manufactured by:
9PRINCIPAL DISPLAY PANEL - 10 mg/5 mL Vial Label
NDC 69794-001-01
Mepsevii
10 mg/5 mL (2 mg/mL)
For Intravenous Infusion
10PRINCIPAL DISPLAY PANEL - 10 mg/5 mL Vial Carton
NDC 69794-001-01
Mepsevii
Injection
10 mg/5 mL (2 mg/mL)
For Intravenous Infusion
Single-Dose Vial
Discard Unused Portion
Package contains one vial
Rx only
ultragenyx


