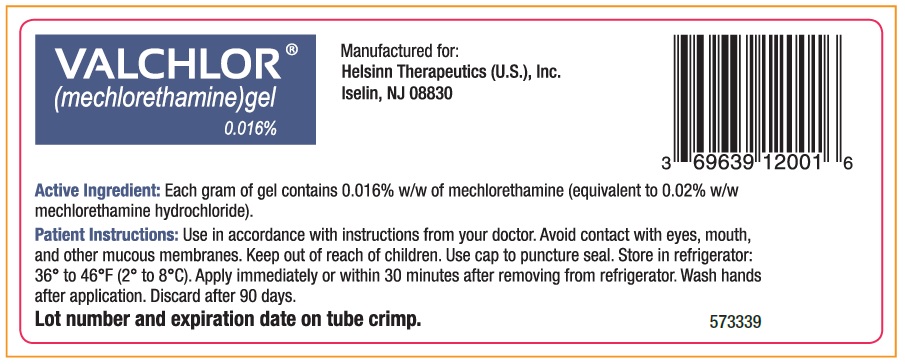
Valchlor
What is Valchlor (Mechlorethamine)?
Approved To Treat
Related Clinical Trials
Objective: * To determine the safety of one intravenous infusion of escalating doses of autologous, CD123-CAR T cells in patients (≤21 years) with recurrent/refractory CD123+ disease (AML/MDS, B-ALL, T-ALL or BPDCN) after lymphodepleting chemotherapy. * To determine the safety of an intravenous infusion of escalating doses of donor derived, CD123-CAR T cells in patients (≤21 years) with recurrent/refractory ...
Summary: 3CAR is being done to investigate an immunotherapy for patients with solid tumors. It is a Phase I clinical trial evaluating the use of autologous T cells genetically engineered to express B7-H3-CARs for patients ≤ 21 years old, with relapsed/refractory B7-H3+ solid tumors. This study will evaluate the safety and maximum tolerated dose of B7-H3-CAR T cells.The purpose of this study is to find the ...
Summary: The purpose of this study is to find out whether N10 chemotherapy is a safe and effective treatment for children with high-risk neuroblastoma.
Related Latest Advances
Brand Information
- Mucosal or eye injury [
- Secondary exposure to VALCHLOR [
- Dermatitis [
- Non-melanoma skin cancer [
Apply a thin film of VALCHLOR once daily to affected areas of the skin [see Dosage and Administration (].
- Apply immediately or within 30 minutes after removal from the refrigerator. Return VALCHLOR to the refrigerator immediately after each use.
- Apply VALCHLOR to completely dry skin at least 4 hours before or 30 minutes after showering or washing. Allow treated areas to dry for 5 to 10 minutes after application before covering with clothing.
- Emollients (moisturizers) may be applied to the treated areas 2 hours before or 2 hours after application of VALCHLOR.
- Occlusive (air or water-tight) dressings should not be used on areas of the skin where VALCHLOR was applied.
Store VALCHLOR refrigerated at temperatures between 36°F - 46°F (2°C - 8°C). Advise patients that adherence to the recommended storage condition will ensure VALCHLOR will work as expected. Patients should consult a pharmacist prior to using VALCHLOR that has been left at room temperature for longer than one hour per day. Unused product should be discarded after 90 days [see How Supplied/Storage and Handling (].
Exposure of the eyes to mechlorethamine causes pain, burns, inflammation, photophobia, and blurred vision. Blindness and severe irreversible eye injury may occur. Should eye contact occur, immediately irrigate for at least 15 minutes with copious amounts of water, normal saline, or a balanced salt ophthalmic irrigating solution, followed by immediate ophthalmologic consultation [see Warnings and Precautions (].
Avoid direct skin contact with VALCHLOR in individuals other than the patient. Risks of secondary exposure include dermatitis, mucosal injury, and secondary cancers. Caregivers who help apply VALCHLOR to patients must wear disposable nitrile gloves when handling VALCHLOR. If secondary exposure occurs to eyes, mouth, or nose, immediately irrigate the exposed area for at least 15 minutes with copious amounts of water. Thoroughly wash affected areas of the skin with soap and water [see Dosage and Administration (].
If patients experience skin irritation after applying VALCHLOR, such as redness, swelling, inflammation, itchiness, blisters, ulceration, or secondary skin infections, instruct patients to discuss with their physician options for changes in the treatment plan. The face, genitalia, anus, or intertriginous skin (skin folds or creases) are at increased risk of skin irritation [see Warnings and Precautions (].
Instruct patients to notify their physician of any new skin lesions and to undergo periodic assessment for signs and symptoms of skin cancer. Non-melanoma skin cancers have been reported in patients receiving the active ingredient in VALCHLOR. Non-melanoma skin cancer may occur at multiple areas, including areas not directly treated with VALCHLOR [see Warnings and Precautions (].
(mechlorethamine) gel
Dispense with Medication Guide