Cosentyx
What is Cosentyx (Secukinumab)?
Living with a chronic inflammatory condition like psoriasis or psoriatic arthritis is more than a physical challenge; it can affect your emotional well-being and daily life. The persistent discomfort, visible symptoms, and joint stiffness can be frustrating, especially when traditional treatments don’t provide enough relief. For many, advanced therapies have opened a new door to managing these complex diseases. One of these options is Cosentyx (secukinumab).
Cosentyx is a modern prescription medication known as a biologic. Biologics are specially engineered proteins made from living cells that are designed to target specific parts of the immune system. Cosentyx belongs to a class of drugs called interleukin-17A (IL-17A) inhibitors. It is not a first-line treatment but is often prescribed for moderate to severe conditions when other therapies have proven insufficient. Understanding how this targeted therapy works is a key step in taking control of your health journey.
What does Cosentyx do?
Cosentyx is approved by the U.S. Food and Drug Administration (FDA) to treat several autoimmune and inflammatory conditions in adults and children, depending on the specific disease.
Its primary uses include:
- Moderate to severe plaque psoriasis: Cosentyx offers significant skin clearance for systemic or phototherapy candidates, reducing redness, scaling, and itching.
- Active psoriatic arthritis (PsA): Cosentyx treats psoriatic arthritis by reducing joint pain, stiffness, and swelling, improving function, and preventing joint damage, alongside treating skin psoriasis.
- Active ankylosing spondylitis (AS): Cosentyx treats inflammatory arthritis of the spine, easing pain and stiffness, and improving mobility.
- Active non-radiographic axial spondyloarthritis (nr-axSpA): A condition similar to AS but without visible joint damage on X-rays.
Clinical trials have demonstrated the effectiveness of Cosentyx. For many patients with plaque psoriasis, studies have shown that a significant number achieved 75% to 90% clearer skin within the first few months of treatment, with results often lasting with continued therapy (Novartis Pharmaceuticals Corporation, 2023). This level of improvement can be life-changing for those who have struggled with persistent symptoms.
How does Cosentyx work?
In a healthy individual, the immune system produces proteins to fight off infections. In autoimmune conditions, this system becomes overactive and mistakenly attacks the body’s own tissues. A key protein involved in this process is called interleukin-17A (IL-17A).
Think of IL-17A as a messenger that sends out constant signals to increase inflammation. In conditions like psoriasis and psoriatic arthritis, the body produces too much IL-17A, which leads to the rapid growth of skin cells (plaques) and inflammation in the joints.
Cosentyx works by specifically targeting and blocking the action of IL-17A. It acts like a precision tool that intercepts and neutralizes this specific inflammatory messenger. By stopping the IL-17A signal, Cosentyx helps to quiet the overactive immune response. This targeted mechanism is important because it calms the specific pathway driving the disease without broadly suppressing the entire immune system, helping to restore balance and reduce symptoms at their source.
Cosentyx side effects
As with any medication, Cosentyx has potential side effects. Your healthcare provider will review these with you and monitor your health to ensure the treatment is safe for you.
The most common side effects are generally mild and may include:
- Cold symptoms (runny nose, sore throat)
- Diarrhea
- Upper respiratory infections
Cosentyx can raise infection risk. Your doctor will screen for TB pre-treatment and advise watching for infection signs like fever, persistent cough, or skin sores.
Serious side effects are less common but require attention. Cosentyx may cause new or worsening inflammatory bowel disease (Crohn’s disease or ulcerative colitis). You should tell your doctor immediately if you experience persistent diarrhea, abdominal pain, or blood in your stool. In rare cases, a serious allergic reaction can occur. Seek emergency medical help if you develop hives, trouble breathing, or swelling of your face, tongue, or throat (Mayo Clinic, 2024).
Cosentyx dosage
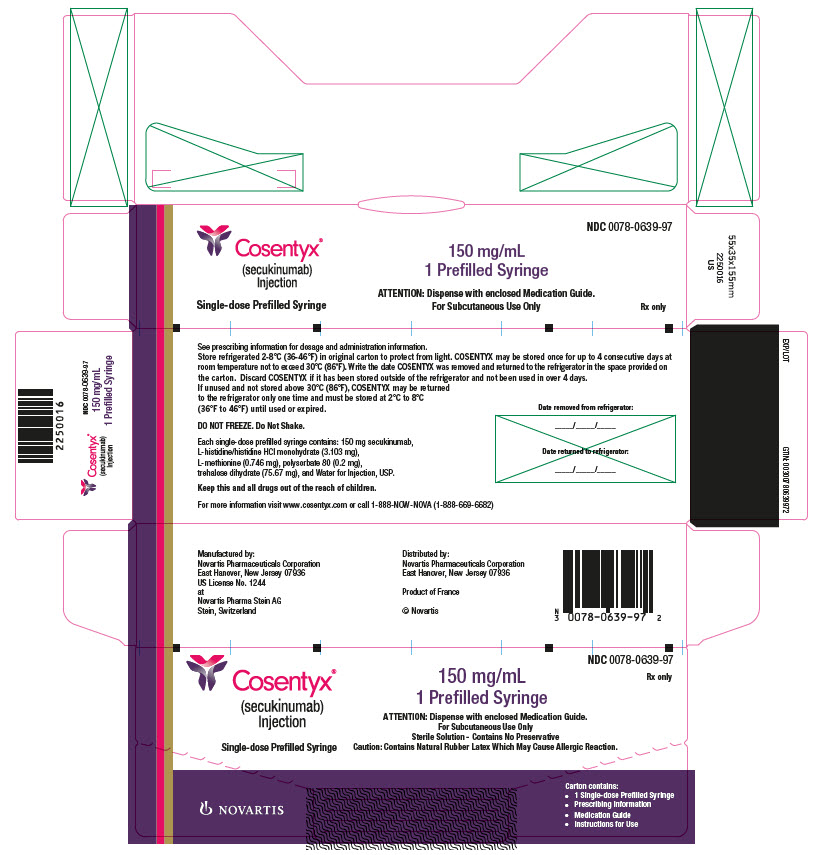
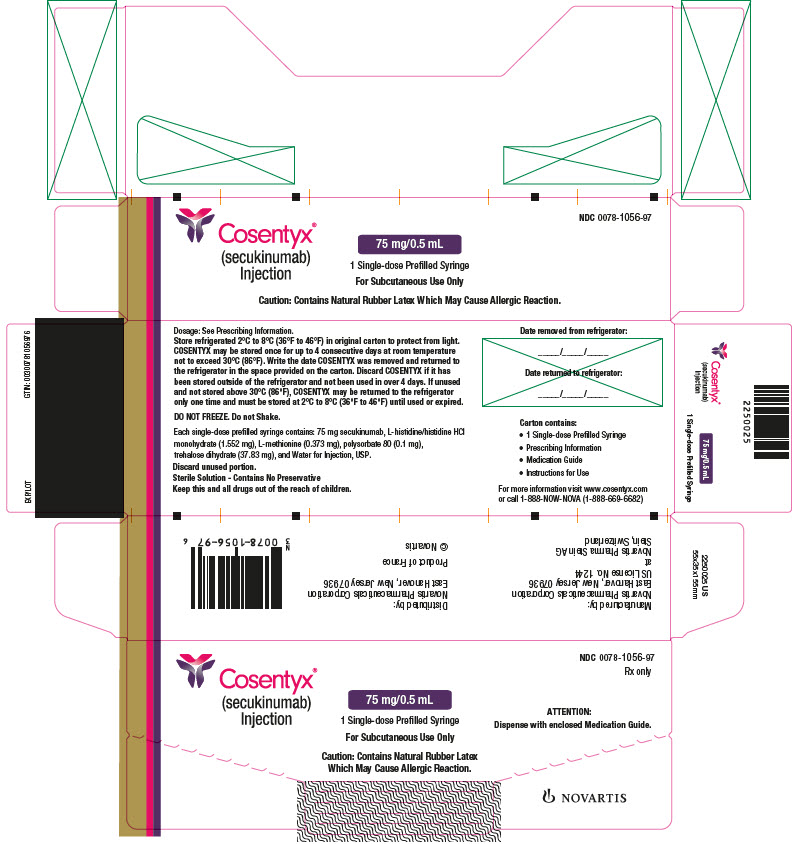
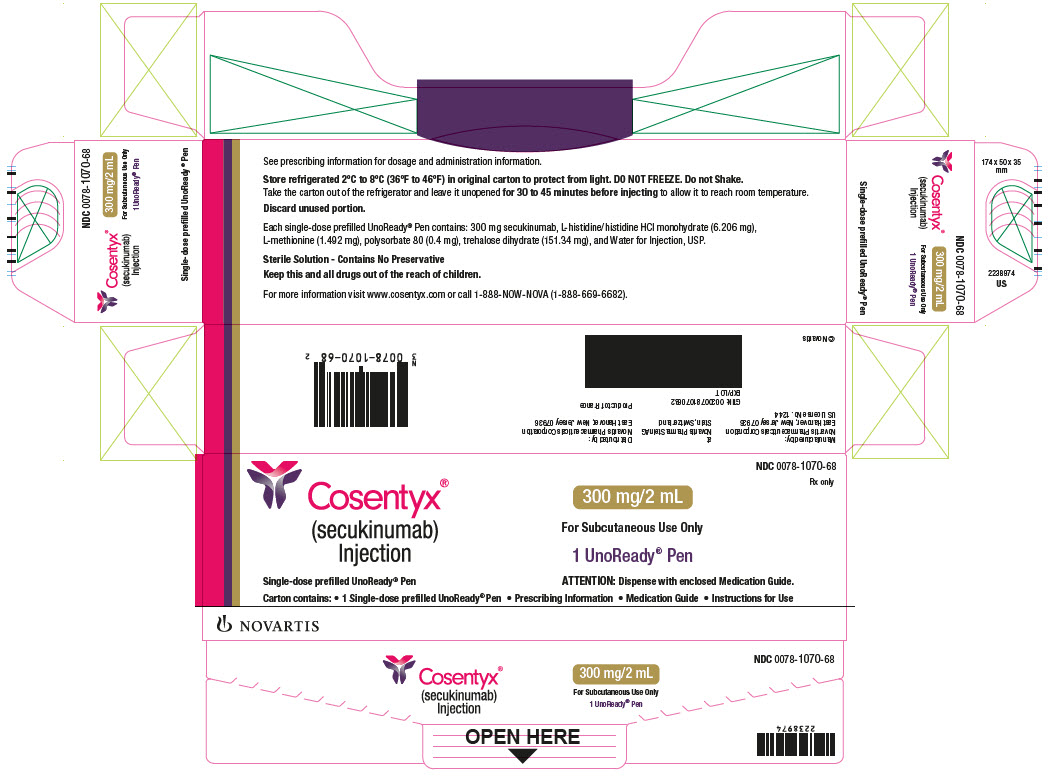
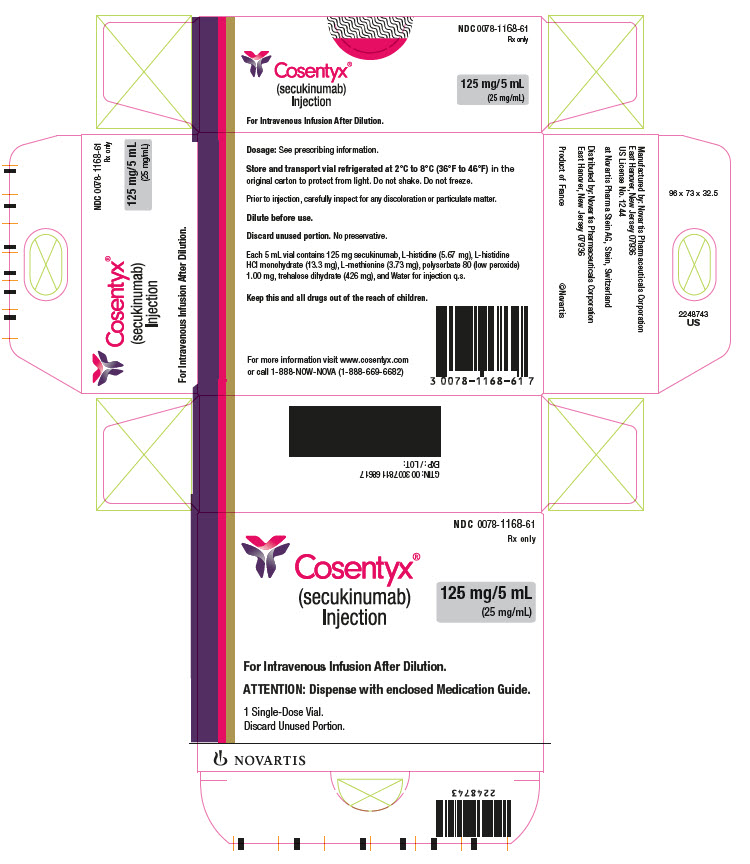
Cosentyx is given as an injection under the skin (subcutaneous injection). It is typically administered using a prefilled syringe, a Sensoready® Pen, or an UnoReady® Pen.
Treatment starts with weekly injections for five weeks (“loading dose”), then switches to a monthly “maintenance dose.” You’ll be taught to self-inject at home.
Before Cosentyx, doctors check for infections like TB. Routine bloodwork isn’t always needed, but regular follow-ups are vital to monitor effectiveness, side effects, and ensure continued suitability.
Does Cosentyx have a generic version?
Currently, there is no generic or biosimilar version of Cosentyx (secukinumab) available in the United States. However, international versions may exist in other markets. Cosentyx is a complex biologic medication, and creating an exact copy (a generic) is not possible.
Instead of generics, biologics have alternatives called “biosimilars.” A biosimilar is a biologic drug that has been shown to be highly similar to an already FDA-approved biologic and has no clinically meaningful differences in terms of safety and effectiveness (FDA, 2023). While biosimilars exist for other biologic drugs, an FDA-approved biosimilar for Cosentyx has not yet been brought to market.
Conclusion
For those living with the challenges of moderate to severe psoriasis, psoriatic arthritis, or other related inflammatory conditions, Cosentyx offers a highly targeted and effective treatment option. By precisely blocking the IL-17A protein, it helps to control the underlying inflammation that drives these diseases, leading to clearer skin, reduced joint pain, and an improved quality of life.
While patient experiences can vary, Cosentyx is a well-established therapy with a clear safety profile. When prescribed and monitored by a qualified healthcare provider, it can be a powerful tool in managing your condition. Working in partnership with your doctor will help you make informed decisions and find the treatment plan that best supports your long-term health and well-being.
References
- Food and Drug Administration (FDA). (2023). Biosimilar and Interchangeable Biologics: More Treatment Choices.
- https://www.fda.gov/consumers/consumer-updates/biosimilar-and-interchangeable-biologics-more-treatment-choices
- Mayo Clinic. (2024). Secukinumab (Subcutaneous Route). https://www.mayoclinic.org/drugs-supplements/secukinumab-subcutaneous-route/side-effects/drg-20150388
- Novartis Pharmaceuticals Corporation. (2023). COSENTYX® (secukinumab) Prescribing Information. U.S. Food and Drug Administration. https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/125504s274lbl.pdf
Approved To Treat
Related Clinical Trials
Summary: ANIMA-R is an observational, prospective, non-interventional, multicenter study to assess real-world effectiveness of secukinumab in the treatment of Hidradenitis Suppurativa (HS).
Summary: Inflammatory diseases may display atypical features making such patients impossible to classify. Management of these cases in daily practice cannot rely on the results of clinical trials nor on guidelines. DNA and RNA mapping have become major tools to understand and sometimes direct the treatment strategy in oncology. This study aims to test whether a precise analysis of molecular pathways in inf...
Summary: The purpose of this extension study is to assess the safety and tolerability of secukinumab when administered long-term in patients with polymyalgia rheumatica.
Related Latest Advances
Brand Information
- 300 mg/2 mL as a clear to opalescent, colorless to slightly yellowish solution in a single-dose UnoReady pen
- 300 mg/2 mL as a clear to opalescent, colorless to slightly yellowish solution in a single-dose prefilled syringe
- 150 mg/mL as a clear to opalescent, colorless to slightly yellowish solution in a single-dose Sensoready pen
- 150 mg/mL as a clear to opalescent, colorless to slightly yellowish solution in a single-dose prefilled syringe
- 75 mg/0.5 mL as a clear to opalescent, colorless to slightly yellowish solution in a single-dose prefilled syringe (for pediatric patients less than 50 kg)
- 125 mg/5 mL as a clear to opalescent, colorless to slightly yellowish solution in a single-dose vial for dilution prior to intravenous infusion (for healthcare professional use only).
- Infections
- Hypersensitivity Reactions
- Inflammatory Bowel Disease
- Eczematous Eruptions
- The first was a randomized, double-blind, placebo and active-controlled, 236-week trial (Trial PsO8) that enrolled 162 pediatric subjects 6 years of age and older, with severe PsO (defined by PASI score ≥ 20, an IGA modified 2011 score of 4, and involving ≥ 10% of the body surface area [BSA]) who were candidates for systemic therapy. The 162 subjects were randomized to receive placebo, a biologic active control, or COSENTYX. In the COSENTYX groups, subjects with body weight (BW) less than 25 kg received 75 mg, subjects with BW 25 to less than 50 kg received either 75 mg or 150 mg (2 times the recommended dose), and subjects with BW of at least 50 kg received either 150 mg or 300 mg (2 times the recommended dose). Subjects were dosed at Weeks 0, 1, 2, 3, and 4 and every 4 weeks thereafter.
- The second trial was a randomized, open-label, 208-week trial (Trial PsO9; NCT03668613) of 84 pediatric subjects 6 years of age and older with moderate to severe PsO (defined by a PASI score ≥ 12, IGA mod 2011 score of ≥ 3, and BSA involvement of ≥ 10% at randomization) who were randomized into two COSENTYX arms [Arm 1: 75 mg for BW < 50 kg or 150 mg for ≥ 50 kg; and Arm 2: 75 mg for BW < 25 kg, 150 mg for BW ≥ 25 kg and < 50 kg, or 300 mg for BW ≥ 50 kg]. Subjects were dosed at Weeks 0, 1, 2, 3, and 4 and every 4 weeks thereafter.
- NDC 0078-1070-68: Carton of one 300 mg/2 mL (300 mg dose) single-dose UnoReady pen (injection)
- NDC 0078-1070-97: Carton of one 300 mg/2 mL (150 mg/mL) single-dose prefilled syringe (injection)
- NDC 0078-0639-41: Carton of two 150 mg/mL (300 mg dose) single-dose Sensoready pens (injection)
- NDC 0078-0639-68: Carton of one 150 mg/mL single-dose Sensoready pen (injection)
- NDC 0078-0639-98: Carton of two 150 mg/mL (300 mg dose) single-dose prefilled syringes (injection)
- NDC 0078-0639-97: Carton of one 150 mg/mL single-dose prefilled syringe (injection)
- NDC 0078-1056-97: Carton of one 75 mg/0.5 mL single-dose prefilled syringe (injection)
- NDC 0078-1168-61: Carton containing one 125 mg/5 mL (25 mg/mL) solution in a single-dose vial for dilution prior to intravenous infusion.
- May be stored for up to 4 days at room temperature not to exceed 30°C (86°F).
- Write the date COSENTYX is removed from and returned to the refrigerator in the space provided on the carton.
- Discard if stored outside of the refrigerator over 4 days.
- May be returned to the refrigerator only one time and must be stored at 2ºC to 8ºC (36ºF to 46ºF) until used or expired.