Brand Name
Betaseron
Generic Name
Beta-1B
View Brand Information FDA approval date: July 09, 2009
Form: Kit
What is Betaseron (Beta-1B)?
BETASERON is indicated for the treatment of relapsing forms of multiple sclerosis , to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in adults. BETASERON is an interferon beta indicated for the treatment of relapsing forms of multiple sclerosis, to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in adults.
Approved To Treat
Save this treatment for later
Not sure about your diagnosis?
Related Clinical Trials
There is no clinical trials being done for this treatment
Related Latest Advances
Brand Information
Betaseron (interferon beta-1b)
1INDICATIONS AND USAGE
BETASERON is indicated for the treatment of relapsing forms of multiple sclerosis (MS), to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in adults.
2DOSAGE FORMS AND STRENGTHS
For injection: 0.3 mg lyophilized powder in a single-dose vial for reconstitution.
3CONTRAINDICATIONS
BETASERON is contraindicated in patients with a history of hypersensitivity to natural or recombinant interferon beta, Albumin (Human), or any other component of the formulation.
4ADVERSE REACTIONS
The following serious adverse reactions are discussed in more details in other sections of labeling:
- Hepatic Injury
- Anaphylaxis and Other Allergic Reactions
- Depression and Suicide
- Congestive Heart Failure
- Injection Site Reactions Including Necrosis
- Leukopenia
- Thrombotic Microangiopathy
- Pulmonary Arterial Hypertension [see Warnings and Precautions (
- Flu-like Symptom Complex
- Seizures
- Drug Induced Lupus Erythematosus
4.1Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions and over varying lengths of time, adverse reaction rates observed in the clinical trials of BETASERON cannot be directly compared to rates in clinical trials of other drugs, and may not reflect the rates observed in practice.
Among 1407 patients with MS treated with BETASERON 0.25 mg every other day (including 1261 patients treated for greater than one year), the most commonly reported adverse reactions (at least 5% more frequent on BETASERON than on placebo) were injection site reaction, lymphopenia, flu-like symptoms, myalgia leukopenia, neutropenia, increased liver enzymes, headache, hypertonia, pain, rash, insomnia, abdominal pain, and asthenia. The most frequently reported adverse reactions resulting in clinical intervention (for example, discontinuation of BETASERON, adjustment in dosage, or the need for concomitant medication to treat an adverse reaction symptom) were depression, flu-like symptom complex, injection site reactions, leukopenia, increased liver enzymes, asthenia, hypertonia, and myasthenia.
Table 2 enumerates adverse reactions and laboratory abnormalities that occurred among patients treated with 0.25 mg of BETASERON every other day by subcutaneous injection in the pooled placebo-controlled trials (Study 1-4) at an incidence that was at least 2% more than that observed in the placebo-treated patients [see Clinical Studies (.
In addition to the Adverse Reactions listed in
Laboratory Abnormalities
In the four clinical trials (Studies 1, 2, 3, and 4), leukopenia was reported in 18% and 6% of patients in BETASERON- and placebo-treated groups, respectively. No patients were withdrawn or dose reduced for neutropenia in Study 1. Three percent (3%) of patients in Studies 2 and 3 experienced leukopenia and were dose-reduced. Other abnormalities included increase of SGPT to greater than five times baseline value (12%), and increase of SGOT to greater than five times baseline value (4%). In Study 1, two patients were dose reduced for increased hepatic enzymes; one continued on treatment and one was ultimately withdrawn. In Studies 2 and 3, 1.5% of BETASERON patients were dose-reduced or interrupted treatment for increased hepatic enzymes. In Study 4, 1.7% of patients were withdrawn from treatment due to increased hepatic enzymes, two of them after a dose reduction. In Studies 1-4, nine (0.6%) patients were withdrawn from treatment with BETASERON for any laboratory abnormality, including four (0.3%) patients following dose reduction.
4.2Immunogenicity
As with all therapeutic proteins, there is a potential for immunogenicity. Serum samples were monitored for the development of antibodies to BETASERON during Study 1. In patients receiving 0.25 mg every other day 56/124 (45%) were found to have serum neutralizing activity at one or more of the time points tested. In Study 4, neutralizing activity was measured every 6 months and at end of study. At individual visits after start of therapy, activity was observed in 17% up to 25% of the BETASERON-treated patients. Such neutralizing activity was measured at least once in 75 (30%) out of 251 BETASERON patients who provided samples during treatment phase; of these, 17 (23%) converted to negative status later in the study. Based on all the available evidence, the relationship between antibody formation and clinical safety or efficacy is not known.
These data reflect the percentage of patients whose test results were considered positive for antibodies to BETASERON using a biological neutralization assay that measures the ability of immune sera to inhibit the production of the interferon-inducible protein, MxA. Neutralization assays are highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of neutralizing activity in an assay may be influenced by several factors including sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to BETASERON with the incidence of antibodies to other products may be misleading.
Anaphylactic reactions have been reported with the use of BETASERON
4.3Postmarketing Experience
The following adverse reactions have been identified during postapproval use of BETASERON. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Blood and lymphatic system disorders: Anemia, Thrombocytopenia, Hemolytic anemia
Endocrine disorders: Hypothyroidism, Hyperthyroidism, Thyroid dysfunction
Metabolism and nutrition disorders: Triglyceride increased, Anorexia, Weight decrease, Weight increase
Psychiatric disorders: Anxiety, Confusion, Emotional lability
Nervous system disorders: Convulsion, Dizziness, Psychotic symptoms
Cardiac disorders: Cardiomyopathy, Palpitations, Tachycardia
Vascular disorders: Vasodilatation
Respiratory, thoracic and mediastinal disorders: Bronchospasm, Pulmonary Arterial Hypertension
Gastrointestinal disorders: Diarrhea, Nausea, Pancreatitis, Vomiting
Hepatobiliary disorders: Hepatitis, Gamma GT increased
Skin and subcutaneous tissue disorders: Alopecia, Pruritus, Skin discoloration, Urticaria
Musculoskeletal and connective tissue disorders: Arthralgia
Reproductive system and breast disorder: Menorrhagia
General disorders and administration site conditions: Fatal capillary leak syndrome1
1The administration of cytokines to patients with a pre-existing monoclonal gammopathy has been associated with the development of this syndrome.
5DESCRIPTION
Interferon beta-1b is a purified, sterile, lyophilized protein product produced by recombinant DNA techniques. Interferon beta-1b is manufactured by bacterial fermentation of a strain of Escherichia coli that bears a genetically engineered plasmid containing the gene for human interferon betaser17. The native gene was obtained from human fibroblasts and altered in a way that substitutes serine for the cysteine residue found at position 17. Interferon beta-1b has 165 amino acids and an approximate molecular weight of 18,500 daltons. It does not include the carbohydrate side chains found in the natural material.
The specific activity of BETASERON is approximately 32 million international units (IU)/mg interferon beta-1b. Each vial contains 0.3 mg of interferon beta-1b. The unit measurement is derived by comparing the antiviral activity of the product to the World Health Organization (WHO) reference standard of recombinant human interferon beta. Mannitol, USP and Albumin (Human), USP (15 mg each/vial) are added as stabilizers.
Lyophilized BETASERON is a sterile, white to off-white powder, for subcutaneous injection after reconstitution with the diluent supplied (Sodium Chloride, 0.54% Solution). Albumin (Human) USP and Mannitol, USP (15 mg each/vial) are added as stabilizers.
6CLINICAL STUDIES
The clinical effects of BETASERON were studied in four randomized, multicenter, double-blind, placebo-controlled studies in patients with multiple sclerosis (Studies 1, 2, 3, and 4).
Patients with Relapsing-Remitting Multiple Sclerosis
The effectiveness of BETASERON in relapsing-remitting MS (RRMS) was evaluated in a double-blind, multiclinic, randomized, parallel, placebo controlled clinical study of two years duration (Study 1). The study enrolled MS patients, aged 18 to 50, who were ambulatory [Kurtzke Expanded Disability Status Scale (EDSS) of ≤ 5.5 – score 5.5 is ambulatory for 100 meters, disability precludes full daily activities], exhibited a relapsing-remitting clinical course, met Poser's criteria for clinically definite and/or laboratory supported definite MS and had experienced at least two exacerbations over two years preceding the trial without exacerbation in the preceding month. The EDSS score is a method of quantifying disability in patients with MS and ranges from 0 (normal neurologic exam) to 10 (death due to MS). Patients who had received prior immunosuppressant therapy were excluded.
An exacerbation was defined as the appearance of a new clinical sign/symptom or the clinical worsening of a previous sign/symptom (one that had been stable for at least 30 days) that persisted for a minimum of 24 hours.
Patients selected for study were randomized to treatment with either placebo (N=123), 0.05 mg of BETASERON (N=125), or 0.25 mg of BETASERON (N=124) self-administered subcutaneously every other day. Outcome based on the 372 randomized patients was evaluated after two years.
Patients who required more than three 28-day courses of corticosteroids were removed from the study. Minor analgesics (acetaminophen, codeine), antidepressants, and oral baclofen were allowed ad libitum, but chronic nonsteroidal anti-inflammatory drug (NSAID) use was not allowed.
The primary protocol-defined outcome measures were 1) frequency of exacerbations per patient and 2) proportion of exacerbation free patients. A number of secondary clinical and magnetic resonance imaging (MRI) measures were also employed. All patients underwent annual T2 MRI imaging and a subset of 52 patients at one site had MRIs performed every six weeks for assessment of new or expanding lesions.
The study results are shown in
Of the 372 RRMS patients randomized, 72 (19%) failed to complete two full years on their assigned treatments.
Over the two-year period in Study 1, there were 25 MS-related hospitalizations in the 0.25 mg BETASERON-treated group compared to 48 hospitalizations in the placebo group. In comparison, non-MS hospitalizations were evenly distributed among the groups, with 16 in the 0.25 mg BETASERON group and 15 in the placebo group. The average number of days of MS-related steroid use was 41 days in the 0.25 mg BETASERON group and 55 days in the placebo group (p=0.004).
MRI data were also analyzed for patients in this study. A frequency distribution of the observed percent changes in MRI area at the end of two years was obtained by grouping the percentages in successive intervals of equal width.
Figure
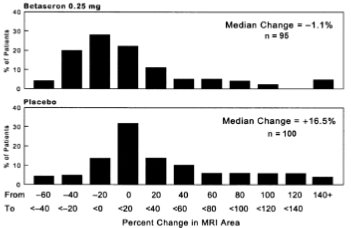
In an evaluation of frequent MRI scans (every six weeks) on 52 patients at one site in Study 1, the percent of scans with new or expanding lesions was 29% in the placebo group and 6% in the 0.25 mg treatment group (p=0.006).
Patients with Secondary Progressive Multiple Sclerosis
Studies 2 and 3 were multicenter, randomized, double-blind, placebo controlled trials conducted to assess the effect of BETASERON in patients with secondary progressive MS (SPMS). Study 2 was conducted in Europe and Study 3 was conducted in North America. Both studies enrolled patients with clinically definite or laboratory-supported MS in the secondary progressive phase, and who had evidence of disability progression (both Study 2 and 3) or two relapses (Study 2 only) within the previous two years. Baseline Kurtzke expanded disability status scale (EDSS) scores ranged from 3.0 to 6.5. Patients in Study 2 were randomized to receive BETASERON 0.25 mg (N=360) or placebo (N=358). Patients in Study 3 were randomized to BETASERON 0.25 mg (N=317), BETASERON 0.16 mg/m2 of body surface area (N=314, mean assigned dose 0.3 mg), or placebo (N=308). Test agents were administered subcutaneously, every other day for three years.
The primary outcome measure was progression of disability, defined as a 1.0 point increase in the EDSS score, or a 0.5 point increase for patients with baseline EDSS ≥ 6.0. In Study 2, time to progression in EDSS was longer in the BETASERON treatment group (p=0.005), with estimated annualized rates of progression of 16% and 19% in the BETASERON and placebo groups, respectively. In Study 3, the rates of progression did not differ significantly between treatment groups, with estimated annualized rates of progression of 12%, 14%, and 12% in the BETASERON fixed dose, surface area-adjusted dose, and placebo groups, respectively.
Multiple analyses, including covariate and subset analyses based on sex, age, disease duration, clinical disease activity prior to study enrollment, MRI measures at baseline and early changes in MRI following treatment were evaluated in order to interpret the discordant study results. No demographic or disease-related factors enabled identification of a patient subset where BETASERON treatment was predictably associated with delayed progression of disability.
In Studies 2 and 3, like Study 1, a statistically significant decrease in the incidence of relapses associated with BETASERON treatment was demonstrated. In Study 2, the mean annual relapse rates were 0.42 and 0.63 in the BETASERON and placebo groups, respectively (p<0.001). In Study 3, the mean annual relapse rates were 0.16, 0.20, and 0.28, for the fixed dose, surface area-adjusted dose, and placebo groups, respectively (p<0.02).
MRI endpoints in both Study 2 and Study 3 showed smaller increases in T2 MRI lesion area and decreased number of active MRI lesions in patients in the BETASERON groups compared to the placebo group.
Patients with an Isolated Demyelinating Event and Typical MS Lesions on Brain MRI
In Study 4, 468 patients who had recently (within 60 days) experienced an isolated demyelinating event, and who had lesions typical of multiple sclerosis on brain MRI were randomized to receive either 0.25 mg BETASERON (N = 292) or placebo (N=176) subcutaneously every other day (ratio 5:3). The primary outcome measure was time to development of a second exacerbation with involvement of at least two distinct anatomical regions. Secondary outcomes were brain MRI measures, including the cumulative number of newly active lesions, and the absolute change in T2 lesion volume. Patients were followed for up to two years or until they fulfilled the primary endpoint.
Eight percent of subjects on BETASERON and 6% of subjects on placebo withdrew from the study for a reason other than the development of a second exacerbation. Time to development of a second exacerbation was significantly delayed in patients treated with BETASERON compared to patients treated with placebo (p<0.0001). The Kaplan-Meier estimates of the percentage of patients developing an exacerbation within 24 months were 45% in the placebo group and 28% of the BETASERON group (
Figure
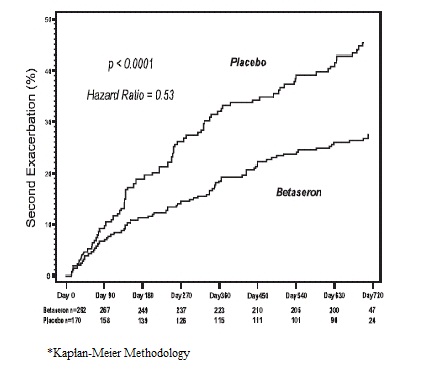
In Study 4, patients treated with BETASERON demonstrated a lower number of newly active lesions during the course of the study. A significant difference between BETASERON and placebo was not seen in the absolute change in T2 lesion volume during the course of the study.
7PATIENT COUNSELING INFORMATION
See FDA-approved patient labeling (Medication Guide and Instructions for Use).
Instruct patients to carefully read the supplied BETASERON Medication Guide and caution patients not to change the BETASERON dose or schedule of administration without medical consultation.
Instruction on Self-Injection Technique and Procedures
Provide appropriate instruction for reconstitution of BETASERON and methods of self-injection, including careful review of the BETASERON Medication Guide. Instruct patients in the use of aseptic technique when administering BETASERON.
Tell patients not to re-use needles or syringes and instruct patients on safe disposal procedures. Advise patients of the importance of rotating areas of injection with each dose, to minimize the likelihood of severe injection site reactions, including necrosis or localized infection
Hepatic Injury
Advise patients that severe hepatic injury, including hepatic failure, has been reported during the use of BETASERON.
Inform patients of symptoms of hepatic dysfunction, and instruct patients to report them immediately to their healthcare provider
Anaphylaxis and Other Allergic Reactions
Advise patients of the symptoms of allergic reactions and anaphylaxis, and instruct patients to seek immediate medical attention if these symptoms occur
Depression and Suicide
Advise patients that depression and suicidal ideation have been reported during the use of BETASERON. Inform patients of the symptoms of depression or suicidal ideation, and instruct patients to report them immediately to their healthcare provider
Congestive Heart Failure
Advise patients that worsening of pre-existing congestive heart failure have been reported in patients using BETASERON.
Advise patients of symptoms of worsening cardiac condition, and instruct patients to report them immediately to their healthcare provider
Injection Site Reactions Including Necrosis
Advise patients that injection site reactions occur in most patients treated with BETASERON, and that injection site necrosis may occur at one or multiple sites. Instruct patients to promptly report any break in the skin, which may be associated with blue-black discoloration, swelling, or drainage of fluid from the injection site, prior to continuing their BETASERON therapy
Pulmonary Arterial Hypertension
Inform patients that PAH has occurred in patients treated with interferon beta products, including BETASERON. Instruct patients to promptly report any new symptoms such as new or increasing fatigue or shortness of breath to their healthcare provider
Flu-like Symptom Complex
Inform patients that flu-like symptoms are common following initiation of therapy with BETASERON, and that concurrent use of analgesics and/or antipyretics on treatment days may help ameliorate flu-like symptoms associated with BETASERON use
Seizures
Instruct patients to report seizures immediately to their healthcare provider
Pregnancy
Advise patients to notify their healthcare provider if they are pregnant or plan to become pregnant
8Medication Guide
This Medication Guide has been approved by the U.S. Food and Drug Administration Revised: 7/2023
9Instructions for Use
BETASERON
(bay-ta-seer-on)
(bay-ta-seer-on)
interferon beta-1b
Read the Instructions for Use that come with your BETASERON before you start using it and each time you get a refill. There may be new information. This leaflet does not take the place of talking to your healthcare provider about your medical condition or treatment. Before you use BETASERON for the first time, make sure your healthcare provider shows you the right way to use it.
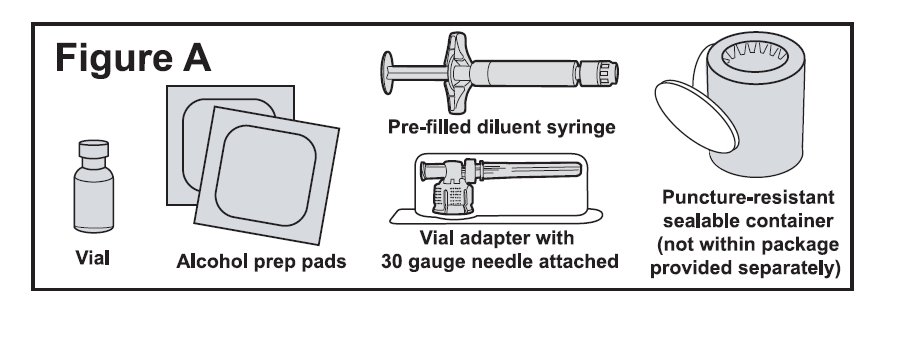
Supplies needed for your BETASERON Injection (See Figure A).
- 1 single-dose carton containing:
- A vial of BETASERON
- A pre-filled diluent syringe
- A vial adapter with a 30-gauge needle attached (in the blister pack)
- 2 alcohol prep pads
Step 1: Preparing for Your BETASERON Injection
- Place the supplies you will need on a clean, flat surface in a well-lit area.
- Check the expiration date on the single-dose carton to make sure that it has not expired.
- Wash your hands thoroughly with soap and water.
- Open the single-dose carton and take out all the contents. Make sure the blister pack containing the vial adapter is sealed. Check to make sure the plastic cap on the pre-filled diluent syringe is firmly attached.
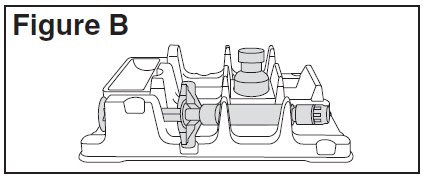
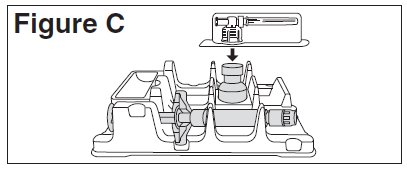
- Remove the tray from the single-dose carton and place it on a flat surface.
- Place the BETASERON vial in the well (vial holder) and place the pre-filled diluent syringe in the U-shaped trough
Step 2: Mixing BETASERON
- Remove the BETASERON vial from the well (vial holder) and take the cap off the vial.
- Place the vial back into the well (vial holder).
- Use an alcohol prep pad to clean the top of the vial. Move the alcohol prep pad in 1 direction. Leave the alcohol prep pad on top of the vial.
- Peel the label off the blister pack with the vial adapter in it. The vial adapter is sterile. Do not remove or touch the vial adapter.
- Remove the alcohol prep pad from the top of the BETASERON vial. Pick up the vial adapter in the blister pack. Turn over the blister pack keeping the vial adapter inside. Put the adapter on top of the BETASERON vial. Push down on the adapter until it pierces the rubber top of the BETASERON vial and snaps in place
- Twist the plastic cap from the pre-filled diluent syringe. Throw away the plastic cap
- Keep the vial adapter attached to the vial and remove the vial from the well (vial holder). Be careful not to pull the vial adapter off the top of the vial.
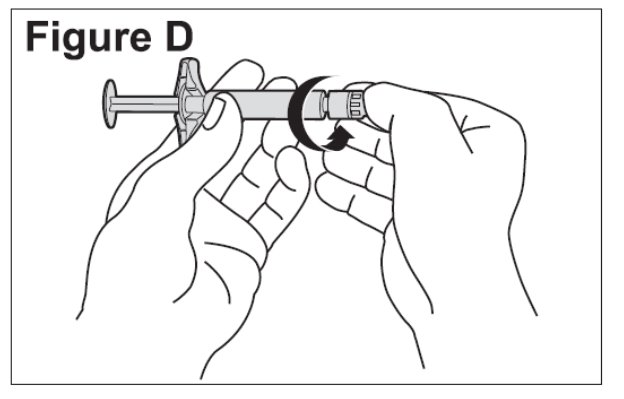
- Connect the pre-filled diluent syringe to the vial adapter by turning clockwise until resistance is felt and the attachment is secure. This forms the syringe assembly
- Slowly push the plunger of the pre-filled diluent syringe all the way in. This will transfer all of the liquid from the syringe into the BETASERON vial
- Gently swirl the vial to completely dissolve the white powder of BETASERON.
- After the powder dissolves, look closely at the solution in the vial. Do not use the solution if it is cloudy or contains particles. It should be clear and colorless.
- Do not use cracked or damaged BETASERON vials. If your vial is cracked or damaged, get a new single-dose carton containing a BETASERON vial, pre-filled diluent syringe, vial adapter and 2 alcohol prep pads. Repeat the steps to prepare your BETASERON dose.
- Contact BETAPLUS, the BETASERON patient support program, at 1-800-788-1467 to obtain a replacement product.
Step 3: Preparing the Injection
You have completed the steps to prepare your BETASERON and are ready for the injection. The injection should be given immediately after mixing and allowing any foam in the solution to settle. If you must wait to give yourself the injection, you may refrigerate the solution and use within 3 hours of mixing your BETASERON.
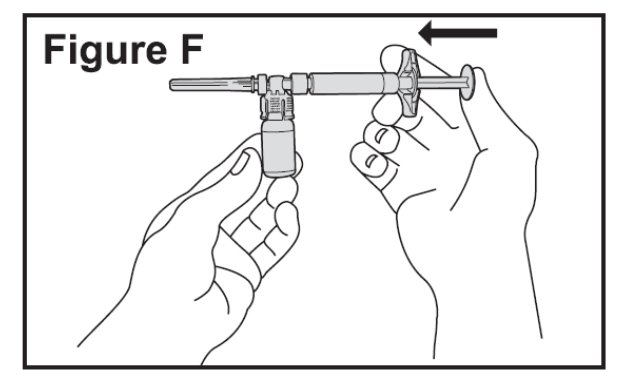
- Push the plunger in and hold it there; then turn the syringe assembly so that the syringe is horizontal and the vial is on top.
- Slowly pull the plunger back to withdraw all the liquid from the BETASERON vial into the syringe
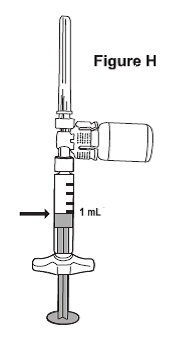
- NOTE: The syringe barrel is marked with numbers from 0.25 mL to 1 mL
- Turn the syringe assembly so that the needle end is pointing up. Remove any air bubbles by tapping the outside of the syringe with your fingers. Slowly push the plunger to the 1 mL mark on the syringe or to the mark that matches the amount of BETASERON prescribed by your healthcare provider
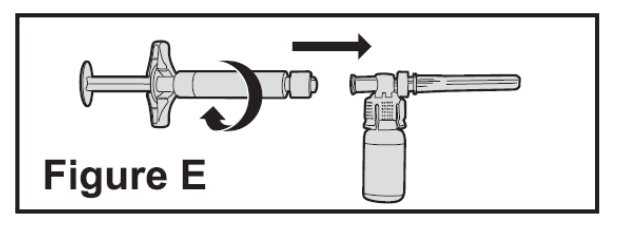
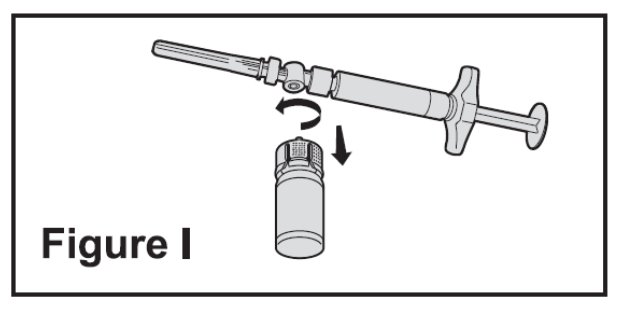
- Turn the syringe assembly so that the vial is at the bottom. Remove the vial adapter and the vial from the syringe by twisting the vial adapter. This will remove the vial adapter and the vial from the syringe, but will leave the needle on the syringe
Step 4: Choosing an Injection Site
- BETASERON (interferon beta-1b) is injected under the skin and into the fat layer between the skin and the muscles (subcutaneous tissue). The best areas for injection are where the skin is loose and soft and away from the joints, nerves, and bones.
- Choose a different site each time you give yourself an injection.
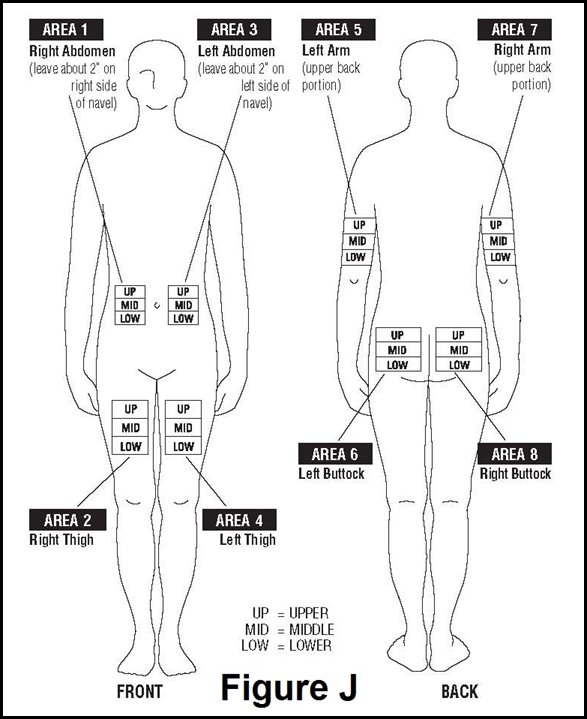
- Do not inject BETASERON in a site where the skin is red, bruised, infected, or scabbed, has broken open, or has lumps, bumps, or pain. Tell your healthcare provider if you find skin conditions like the ones mentioned here or any other unusual-looking areas where you have been given injections.
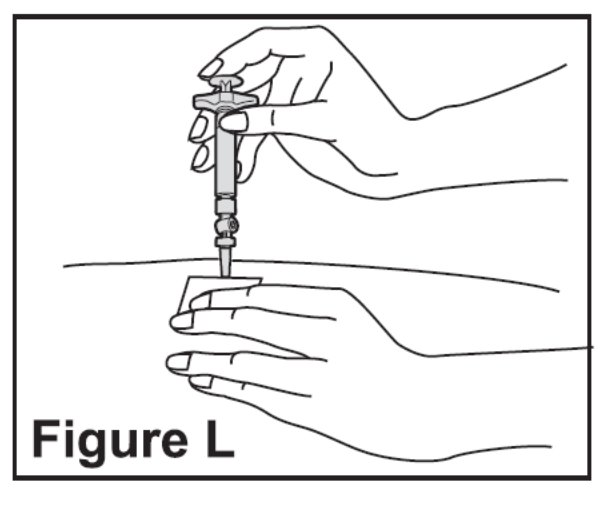
Step 5: Injecting BETASERON
- Using a circular motion, clean the injection site with an alcohol prep pad, starting at the injection site and moving outward. Let the skin area air dry.
- Remove the cap from the needle. Hold the syringe like a pencil or dart in 1 hand.
- Gently pinch the skin around the site with the thumb and forefinger of the other hand
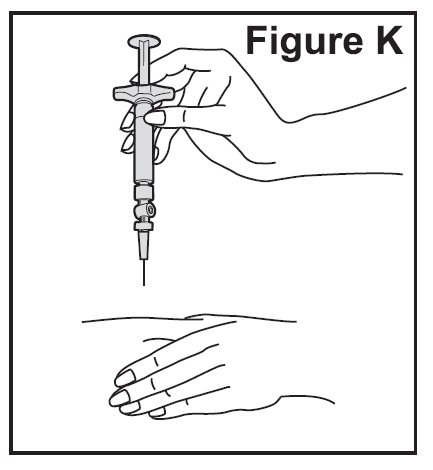
- Slowly push the plunger all the way in until the syringe is empty
- Remove the needle from the skin. Place a dry cotton ball or gauze pad over the injection site. Gently massage the injection site for a few moments with the dry cotton ball or gauze pad. Throw away the syringe in your puncture-proof disposal container.
- Optional Use of BETACONNECT Autoinjector:
Step 6: Disposing of used syringes, needles, and vials
- To prevent needle-stick injury and spread of infection, do not try to re-cap the needle.
- Place used needles, syringes, and vials in a closeable, puncture-resistant container. You may use a sharps container (such as a red biohazard container), hard plastic container (such as a detergent bottle), or metal container (such as an empty coffee can). Do not use glass or clear plastic containers. Ask your healthcare provider for instructions on the right way to throw away (dispose of) the container. There may be state and local laws about how you should throw away used needles and syringes.
- Do not throw used needles, syringes, or vials in your household trash or recycle.
- Throw away any unused medicine. Do not save any unused BETASERON for a future dose.
- Keep the disposal container, needles, syringes, and vials of BETASERON out of the reach of children.
This Instructions for Use has been approved by the U.S. Food and Drug Administration 11/2021
Manufactured for:
Bayer HealthCare Pharmaceuticals Inc.
Manufactured in Austria
U.S. License No. 1778
© 1993 Bayer HealthCare Pharmaceuticals Inc. All rights reserved.


