Prialt
What is Prialt (Ziconotide Acetate)?
Approved To Treat
Top Global Experts
Related Clinical Trials
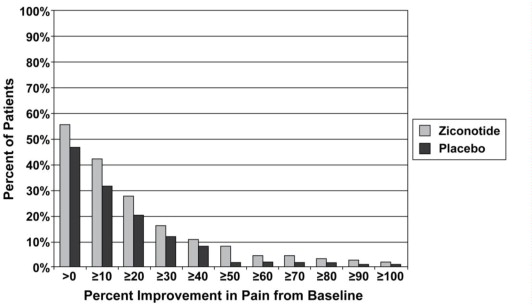
Summary: Ziconotide is a strong analgesic marketed since 2005 in Europe and reserved for the intrathecal route. Its efficacy has been proven in particular by 3 randomized clinical studies. It is particularly effective on neuropathic pain and its main advantages are its power of action, the absence of bone marrow toxicity, and the absence of respiratory depression. In addition, there were no signs of withdr...
Summary: Although ziconotide's marketing authorization does not restrict its use to a given type of pain, the drug has been used mainly in cancer patients. Most data on ziconotide-based intrathecal (IT) treatment has therefore been obtained in this population, for whom the drug's place is clearly documented (national and international recommendations). In contrast the management of non-cancer pain is less ...
Related Latest Advances
Brand Information
- PRIALT is contraindicated in patients with a known hypersensitivity to ziconotide or any of its formulation components.
- PRIALT is contraindicated in patients with any other concomitant treatment or medical condition that would render intrathecal administration hazardous. Contraindications to the use of intrathecal analgesia include the presence of infection at the microinfusion injection site, uncontrolled bleeding diathesis, and spinal canal obstruction that impairs circulation of CSF.
- PRIALT is contraindicated in patients with a pre-existing history of psychosis.
- Advise patients that psychiatric symptoms (paranoia, hostility, mania, depressive, suicidal) and cognitive symptoms (confusion, memory problems, speech disorder) may occur during treatment with PRIALT.
- Caution patients against engaging in hazardous activity requiring complete mental alertness or motor coordination such as operating machinery or driving a motor vehicle during treatment with PRIALT.
- Caution patients about possible combined effects with other CNS-depressant drugs. Dosage adjustments may be necessary when PRIALT is administered with such agents because of the potentially additive effects.
- Advise patients to contact a physician if the patient experiences new or worsening muscle pain, soreness, weakness with or without darkened urine.
- Instruct patients and their caregivers to contact a physician immediately if the patient has any of the following
- A change in mental status (e.g., lethargy, confusion, disorientation, decreased alertness)
- A change in mood, perception (hallucinations, including unusual tactile sensations in the oral cavity)
- Symptoms of depression or suicidal ideation
- Nausea, vomiting, seizures, fever, headache, and/or stiff neck, as these may be symptoms of developing meningitis
- Decreased level of consciousness, unresponsiveness or stupor
- New muscular symptoms (e.g., muscle cramps, myalgias)
- Withdrawal symptoms (e.g., nausea, insomnia, flu-like symptoms) as a result of abruptly discontinuing opioid therapy
- Development of serious skin reaction (e.g., bullous dermatitis, skin ulcers, skin exfoliation)
- Lactation: Advise mothers who have been administered PRIALT to monitor neonates for signs of sedation which may result in respiratory depression and/or feeding problems [