Generic Name
Iothalamate meglumine
Brand Names
Conray, Cysto-Conray
FDA approval date: October 14, 2003
Classification: Radiographic Contrast Agent
Form: Injection
What is Conray (Iothalamate meglumine)?
Conray is indicated for use in excretory urography, cerebral angiography, peripheral arteriography, venography, arthrography, direct cholangiography, endoscopic retrograde cholangiopancreatography, contrast enhancement of computed tomographic brain images, cranial computerized angiotomography, intravenous digital subtraction angiography and arterial digital subtraction angiography. Conray may also be used for enhancement of computed tomographic scans performed for detection and evaluation of lesions in the liver, pancreas, kidneys, abdominal aorta, mediastinum, abdominal cavity and retroperitoneal space. Continuous or multiple scans separated by intervals of 1 to 3 seconds during the first 30 to 90 seconds post-injection of the contrast medium may provide enhancement of diagnostic significance, and may be of benefit in establishing diagnoses of certain lesions in these sites with greater assurance than is possible with CT alone, and in supplying additional features of the lesions. In other cases, the contrast agent may allow visualization of lesions not seen with CT alone, or may help to define suspicious lesions seen with unenhanced CT. Subsets of patients in whom delayed body CT scans might be helpful have not been identified. Inconsistent results have been reported and abnormal and normal tissues may be isodense during the time frame used for delayed CT scanning. The risks of such indiscriminate use of contrast media are well known and such use is not recommended. At present, consistent results have been documented using dynamic CT techniques only.
Approved To Treat
Top Global Experts
Save this treatment for later
Not sure about your diagnosis?
Related Clinical Trials
There is no clinical trials being done for this treatment
Related Latest Advances
Brand Information
Conray (iothalamate meglumine)
1DESCRIPTION
Conray is a sterile aqueous solution intended for use as a diagnostic radiopaque medium. Conray contains 60% w/v iothalamate meglumine, which is 1-deoxy-1-(methylamino)-D-glucitol 5-acetamido-2,4,6 triiodo-N-methylisophthalamate (salt), and has the following structural formula:
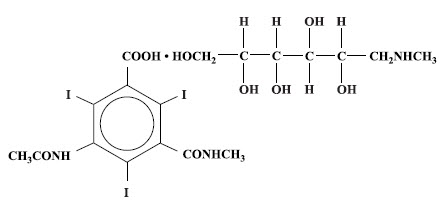
Each milliliter contains 600 mg of iothalamate meglumine, 0.09 mg edetate calcium disodium as a stabilizer and 0.125 mg of monobasic sodium phosphate as a buffer. The solution provides 28.2% (282 mg/mL) organically bound iodine. Conray has an osmolarity of approximately 1000 mOsmol per liter, an osmolality of approximately 1400 mOsmol per kilogram and is, therefore, hypertonic under conditions of use. The viscosity (cps) is approximately 6 at 25°C and 4 at 37°C. The pH is 6.5 to 7.7.
Conray is a clear solution containing no undissolved solids. Crystallization does not occur at normal room temperatures. It is supplied in containers from which the air has been displaced by nitrogen.
2CLINICAL PHARMACOLOGY
Following intravascular injection, Conray is rapidly transported through the circulatory system to the kidneys and is excreted unchanged in the urine by glomerular filtration. The pharmacokinetics of intravascularly administered radiopaque contrast media are usually best described by a two compartment model with a rapid alpha phase for drug distribution and a slower beta phase for drug elimination. In patients with normal renal function, the alpha and beta half-lives of Conray were approximately 10 and 90 minutes, respectively.
Angiography may be performed following intravascular injection which will permit visualization until significant hemodilution occurs.
Renal accumulation is sufficiently rapid that maximum radiographic density in the calyces and pelves occurs, in most instances, about 3 to 8 minutes after injection. In patients with impaired renal function, diagnostic opacification frequently is achieved only after prolonged periods.
Injectable iodinated contrast agents are excreted either through the kidneys or through the liver. These two excretory pathways are not mutually exclusive, but the main route of excretion seems to be related to the affinity of the contrast medium for serum albumin. Iothalamate salts are poorly bound to serum albumin, and are excreted mainly through the kidneys.
The liver and small intestine provide the major alternate route of excretion. In patients with severe renal impairment, the excretion of this contrast medium through the gallbladder and into the small intestine sharply increases.
Iothalamate salts cross the placental barrier in humans and are excreted unchanged in human milk.
The biliary system, pancreatic duct or joint spaces may be visualized by the direct injection of contrast medium into the region to be studied.
2.1CT Scanning of the Head
When used for contrast enhancement in computed tomographic brain scanning, the degree of enhancement is directly related to the amount of iodine administered. Rapid injection of the entire dose yields peak blood iodine concentrations immediately following the injection, which fall rapidly over the next five to ten minutes. This can be accounted for by the dilution in the vascular and extracellular fluid compartments which causes an initial sharp fall in plasma concentration. Equilibration with the extracellular compartments is reached by about ten minutes; thereafter, the fall becomes exponential. Maximum contrast enhancement frequently occurs after peak blood iodine levels are reached. The delay in maximum contrast enhancement can range from five to forty minutes, depending on the peak iodine levels achieved and the cell type of the lesion. This lag suggests that the contrast enhancement of the image is at least in part dependent on the accumulation of iodine within the lesion and outside the blood pool.
In brain scanning, the contrast medium (Conray) does not accumulate in normal brain tissue due to the presence of the “blood brain barrier.” The increase in x-ray absorption in the normal brain is due to the presence of the contrast agent within the blood pool. A break in the blood brain barrier, such as occurs in malignant tumors of the brain, allows accumulation of contrast medium within the interstitial tumor tissue; adjacent normal brain tissue does not contain the contrast medium.
The image enhancement of non-tumoral lesions, such as arteriovenous malformations and aneurysms, is dependent on the iodine content of the circulating blood pool.
When used for cranial computerized angiotomography, rapid bolus injection and/or infusion combined with rapid CT scanning will provide clear delineation of the cerebral vessels.
2.2CT Scanning of the Body
In non-neural tissues (during CT of the body), Conray diffuses rapidly from the vascular to the extra-vascular space. Increase in x-ray absorption is related to blood flow, concentration of the contrast medium and extraction of the contrast medium by interstitial tissue, since no barrier exists; contrast enhancement is thus due to the relative differences in extra-vascular diffusion between normal and abnormal tissue, a situation quite different than that in the brain.
The pharmacokinetics of Conray in normal and abnormal tissues has been shown to be variable.
Enhancement of CT with Conray may be of benefit in establishing diagnoses of certain lesions in some sites with greater assurance than is possible with unenhanced CT and in supplying additional features of the lesions. In other cases, the contrast medium may allow visualization of lesions not seen with CT alone or may help to define suspicious lesions seen with unenhanced CT.
Contrast enhancement appears to be greatest within the 30 to 90 seconds after bolus administration of the contrast agent, and after intra-arterial, rather than intravenous, administration. Therefore, the use of a continuous scanning technique (a series of 2 to 3 second scans beginning at the injection - dynamic CT scanning) may improve enhancement and diagnostic assessment of tumors and other lesions, such as an abscess, occasionally revealing more extensive disease. A cyst, or similar non-vascularized lesion, may be distinguished from vascularized solid lesions by comparing enhanced and unenhanced scans; non-vascularized lesions show no change in CT number, whereas vascularized lesions would show an increase. The latter might be benign, malignant or normal, but it is unlikely that it would be a cyst, hematoma, or other non-vascularized lesion.
Because
3INDICATIONS AND USAGE
Conray is indicated for use in excretory urography, cerebral angiography, peripheral arteriography, venography, arthrography, direct cholangiography, endoscopic retrograde cholangiopancreatography, contrast enhancement of computed tomographic brain images, cranial computerized angiotomography, intravenous digital subtraction angiography and arterial digital subtraction angiography.
Conray may also be used for enhancement of computed tomographic scans performed for detection and evaluation of lesions in the liver, pancreas, kidneys, abdominal aorta, mediastinum, abdominal cavity and retroperitoneal space. Continuous or multiple scans separated by intervals of 1 to 3 seconds during the first 30 to 90 seconds post-injection of the contrast medium (dynamic CT scanning) may provide enhancement of diagnostic significance, and may be of benefit in establishing diagnoses of certain lesions in these sites with greater assurance than is possible with CT alone, and in supplying additional features of the lesions. In other cases, the contrast agent may allow visualization of lesions not seen with CT alone, or may help to define suspicious lesions seen with unenhanced CT (see
4CONTRAINDICATIONS
Refer to PRECAUTIONS, General, concerning hypersensitivity. Conray should not be used for myelography. Arthrography should not be performed if infection is present in or near the joint. Percutaneous transhepatic cholangiography is contraindicated in patients with coagulation defects and prolonged prothrombin times. Endoscopic retrograde cholangiopancreatography is contraindicated during an acute attack of pancreatitis or during severe clinically evident cholangitis and in patients in whom endoscopy is prohibited.
5ADVERSE REACTIONS
Adverse reactions to injectable contrast media fall into two categories: chemotoxic reactions and idiosyncratic reactions.
Chemotoxic reactions result from the physio-chemical properties of the contrast media, the dose and speed of injection. All hemodynamic disturbances and injuries to organs or vessels perfused by the contrast medium are included in this category.
Idiosyncratic reactions include all other reactions. They occur more frequently in patients 20 to 40 years old. Idiosyncratic reactions may or may not be dependent on the amount of dose injected, the speed of injection, the mode of injection and the radiographic procedure. Idiosyncratic reactions are subdivided into minor, intermediate and severe. The minor reactions are self-limited and of short duration; the severe reactions are life-threatening and treatment is urgent and mandatory.
Fatalities have been reported following the administration of iodine-containing contrast agents. Based upon clinical literature, the incidence of death is reported to range from one in 10,000 (0.01 percent) to less than one in 100,000 (0.001 percent).
The following adverse reactions have been observed in conjunction with the use of iodine-containing contrast agents.
The most frequent adverse reactions are nausea, vomiting, facial flush and a feeling of body warmth. These are usually of brief duration. Other reactions include the following:
6OVERDOSAGE
Overdosage may occur. The adverse effects of overdosage are life-threatening and affect mainly the pulmonary and cardiovascular system. The symptoms may include cyanosis, bradycardia, acidosis, pulmonary hemorrhage, convulsions, coma and cardiac arrest. Treatment of an overdose is directed toward the support of all vital functions and prompt institution of symptomatic therapy.
Iothalamate salts are dialyzable.
The intravenous LD
7DOSAGE AND ADMINISTRATION
It is advisable that Conray be at or close to body temperature when injected.
The patient should be instructed to omit the meal that precedes the examination. Appropriate premedication, which may include a barbiturate, tranquilizer or analgesic drug, may be administered prior to the examination.
A preliminary film is recommended to check the position of the patient and the x-ray exposure factors.
If a minor reaction occurs during administration, the injection should be slowed or stopped until the reaction has subsided. If a major reaction occurs, the injection should be discontinued immediately.
Under no circumstances should either corticosteroids or antihistamines be mixed in the same syringe with the contrast medium because of a potential for chemical incompatibility.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration.
8EXCRETORY UROGRAPHY
Following intravenous injection, Conray is rapidly excreted by the kidneys. Conray may be visualized in the renal parenchyma 30 seconds following bolus injection. Maximum radiographic density in the calyces and pelves occurs in most instances within 3 to 8 minutes after injection. In patients with severe renal impairment contrast visualization may be substantially delayed.
8.1Patient Preparation
Appropriate preparation of the patient is important for optimal visualization. A low residue diet is recommended for the day preceding the examination and a laxative is given the evening before the examination, unless contraindicated.
8.2Precautions
Infants and small children should not have any fluid restrictions prior to excretory urography. Injections of Conray represent an osmotic load which, if superimposed on increased serum osmolality due to partial dehydration, may magnify hypertonic dehydration (see
8.3Adverse Reactions
See section on general
8.4Usual Dosage
Adults - The usual dose is 30 to 60 mL. Children 14 years of age and over, of average weight, may receive the adult dose. The total dose is normally injected within 30 to 90 seconds. Higher dosage may be indicated to achieve optimum results in instances where poor visualization may be anticipated (e.g., elderly patients or patients with impaired renal function). When nephrograms and/or sequential urograms are desired, the total dose should be rapidly injected, normally within 15 to 30 seconds.
The dosage for children is reduced in proportion to age and body weight. The following approximate schedule is recommended for infants and children, based on a dosage of about 0.5 mL/kg of body weight:
9CEREBRAL ANGIOGRAPHY
Conray may be used to visualize the cerebral vasculature by any of the accepted techniques.
9.1Patient Preparation
Cerebral angiography is normally performed with local or general anesthesia (see
A preliminary radiograph is usually made prior to injection of the contrast agent.
9.2Precautions
In addition to the general precautions previously described, cerebral angiography should be performed with special caution in patients with advanced arteriosclerosis, severe hypertension, cardiac decompensation, senility, recent cerebral thrombosis or embolism, and migraine.
9.3Adverse Reactions
The major sources of cerebral arteriographic adverse reactions appear to be related to repeated injections of the contrast material, administration of doses higher than those recommended, the presence of occlusive atherosclerotic vascular disease and the method and technique of injection.
Adverse reactions are normally mild and transient. A feeling of warmth in the face and neck is frequently experienced. Infrequently, a more severe burning discomfort is observed.
Serious neurological reactions that have been associated with cerebral angiography and not listed under the general Adverse Reactions include stroke, amnesia and respiratory difficulties.
Cardiovascular reactions that may occur with some frequency are bradycardia and decrease in systemic blood pressure. The blood pressure change is transient and usually requires no treatment.
9.4Usual Dosage
The usual dosage employed varies with the site and method of injection and the age, condition and weight of the patient. In adults, carotid and vertebral angiography, by either the percutaneous needle or catheter methods, is usually performed with a single rapid injection of 6 to 10 mL. Additional injections are made as indicated. Retrograde brachial cerebral angiography, in adults, is usually performed with a single rapid injection of 35 to 50 mL into the right brachial artery. Other dosages may be employed depending upon the vessel injected and the procedure followed. The dose for children is reduced in approximate proportion to age and body weight.
10PERIPHERAL ARTERIOGRAPHY AND VENOGRAPHY
Conray may be injected to visualize the arterial and venous peripheral circulation. Arteriograms of the upper and lower extremities may be obtained by any of the established techniques. Most frequently, a percutaneous injection is made into the brachial artery in the arm or the femoral artery in the leg. Venograms are obtained by injection into an appropriate vein in the upper and lower extremity.
10.1Patient Preparation
The procedure is normally performed with local or general anesthesia (see
A preliminary radiograph is usually made prior to the injection of the contrast agent.
10.2Precautions
In addition to the general precautions previously described, moderate decreases in blood pressure occur frequently with intra-arterial (brachial) injections. This change is usually transient and requires no treatment; however, the blood pressure should be monitored for approximately ten minutes following injection. Special care is required when venography is performed in patients with suspected thrombosis, phlebitis, severe ischemic disease, local infection or a totally obstructed venous system. In the presence of venous stasis, vein irrigation with normal saline should be considered following the procedure. Venography is optimally performed with a more dilute solution such as Conray 43 (Iothalamate Meglumine Injection USP 43%).
Extreme caution during injection of the contrast agent is necessary to avoid extravasation and fluoroscopy is recommended. This is especially important in patients with severe arterial or venous disease.
10.3Adverse Reactions
In addition to the general adverse reactions previously described, hemorrhage and thrombosis have occurred at the puncture site of the percutaneous injection. Brachial plexus injury has been reported following axillary artery injection. Thrombophlebitis, syncope and very rare cases of gangrene have been reported following venography.
10.4Usual Dosage
Peripheral Arteriography: In adults a single rapid injection of 20 to 40 mL is normally sufficient to visualize the entire extremity. The dose for children is reduced in proportion to body weight. Venography: The usual dose for adults is a single rapid injection of 20 to 40 mL. The dose for children is reduced in proportion to body weight. Following the procedure, the venous system should be flushed with either 5% dextrose in water (D5W) or normal saline (Sodium Chloride Injection USP) or the contrast medium should be removed by leg massage and/or leg elevation.
11ENDOSCOPIC RETROGRADE CHOLANGIOPANCREATOGRAPHY
Endoscopic retrograde cholangiopancreatography (ERCP) is indicated in carefully selected patients with known or suspected pancreatic or biliary tract disease when other diagnostic procedures have failed to provide the necessary diagnostic information. Prior to the development of ERCP, x-ray examination of the pancreatic ducts could only be obtained at laparotomy.
11.1Precautions
Endoscopic retrograde cholangiopancreatography should only be performed by personnel skilled and experienced with the procedure, and careful attention to technique is essential for the success and safety of the procedure. Fluoroscopy is mandatory during injection to prevent over distention of the duct systems.
11.2Adverse Reactions
Adverse reactions that have occurred which are attributable to either the procedure or to Conray, include nausea, vomiting, fever, severe abdominal pain, duodenal wall intravasation, septicemia, pancreatitis and perforation of the common bile duct associated with pathology.
11.3Dosage and Administration
The procedure is usually performed following pharyngeal anesthesia and analgesic or sedative premedication. Duodenal motility may be controlled in patients with active duodenal peristalsis with an appropriate antiperistaltic agent.
The contrast medium should be injected slowly under fluoroscopic control employing the minimal dose that is adequate to visualize the common bile duct, the pancreatic duct, or both duct systems. The dosage will vary greatly depending on the pathological findings and can range from 10 to 100 mL for visualization of the common bile duct; and from 2 to 10 mL for visualization of the pancreatic duct.
Following the procedure, the patient should be kept under close observation for 24 hours.
12CRANIAL COMPUTERIZED ANGIOTOMOGRAPHY
Conray may be administered for cranial computerized angiotomography when necessary to visualize the cerebral vessels to detect cerebrovascular lesions and to evaluate the anatomical relationship between the cerebral blood vessels and other parenchymal or space occupying lesions.
12.1Usual Dosage
Conray may be administered by intravenous bolus injection, or by bolus injection followed by rapid infusion.
For bolus injection, the usual dose in adults and children is 0.5 to 1.0 mL/kg at an injection rate of 2 mL/second with scanning begun immediately after administration. This dose may be repeated as necessary. The total dose per procedure should not exceed 200 mL, and in children the total dose is reduced in approximate proportion to age and body weight.
In adults, when the combination bolus and infusion technique is used, a 50 mL bolus injection followed by a rapid infusion of 150 mL may be given or a 100 mL bolus injection followed by a rapid infusion of 100 mL may be used. Scanning is begun immediately after the bolus administration. In children, the dose is reduced in approximate proportion to age and body weight.
13CONTRAST ENHANCEMENT IN BODY COMPUTED TOMOGRAPHY
Conray may be administered when necessary to visualize vessels and organs in patients undergoing CT of the chest, abdomen and pelvis.
13.1Patient Preparation
No special patient preparation is required for contrast enhancement in body CT. In patients undergoing abdominal or pelvic examination, opacification of the bowel may be valuable in scan interpretation.
13.2Precautions
In addition to the general precautions previously described, it is advisable to ensure that patients are adequately hydrated prior to examination. Patient motion, including respiration, can markedly affect image quality, therefore, patient cooperation is essential. The use of an intravascular contrast medium can obscure tumors in patients undergoing CT evaluation of the liver resulting in a false negative diagnosis. Dynamic CT scanning is the procedure of choice for malignant tumor enhancement (see
13.3Usual Dosage
Conray may be administered by bolus injection, by rapid infusion or by a combination of both.
For vascular opacification, a bolus injection of 25 to 50 mL may be used, repeated as necessary. When prolonged arterial or venous phase enhancement is required and for the enhancement of specific lesions, a rapid infusion of 150 mL may be used. In some instances, a 100 to 150 mL infusion may be employed to define the area of interest followed by bolus injections of 20 to 50 mL to clarify selected scans.
14INTRAVENOUS DIGITAL SUBTRACTION ANGIOGRAPHY
Intravenous digital subtraction angiography (IV DSA) is a radiographic modality which allows dynamic imaging of the arterial system following intravenous injection of iodinated x-ray contrast media through the use of image intensification, enhancement of the iodine signal and digital processing of the image data. Temporal subtraction of the images obtained during the “first arterial pass” of the injected contrast medium injection yield images which are devoid of bone and soft tissue.
Areas that have been most frequently examined by intravenous DSA are the heart, including coronary by-pass grafts; the pulmonary arteries; the arteries of the brachiocephalic circulation; the aortic arch; the abdominal aorta and its major branches including the celiac, mesenterics and renal arteries; the iliac arteries; and the arteries of the extremities.
14.1Patient Preparation
No special patient preparation is required for intravenous digital subtraction angiography. However, it is advisable to ensure that patients are well hydrated prior to examination.
14.2Precautions
In addition to the general precautions previously described, the risks associated with IV DSA are those usually attendant with catheter procedures and include intramural injections, vessel dissection and tissue extravasation. Small test injections of contrast medium made under fluoroscopic observation to ensure the catheter tip is properly positioned, and in the case of peripheral placement that the vein is of adequate size, will reduce this potential.
Patient motion, including respiration and swallowing, can result in marked image degradation yielding non-diagnostic studies. Therefore, patient cooperation is essential.
14.3Adverse Reactions
See section on general
14.4Usual Dosage
Conray may be injected either centrally, into the superior or inferior vena cava, or peripherally into an appropriate arm vein. For central injections, catheters may be introduced at the antecubital fossa into either the basilic or cephalic vein or at the leg into the femoral vein and advanced to the distal segment of the corresponding vena cava. For peripheral injections, the catheter is introduced at the antecubital fossa into the appropriate size arm vein. In order to reduce the potential for extravasation during peripheral injection, a catheter of approximately 20 cm in length should be employed.
Depending on the area to be imaged, the usual dose range is 20 to 40 mL. Injections may be repeated as necessary.
Central catheter injections are usually made with a power injector with an injection rate of between 10 and 30 mL/second. When making peripheral injections, rates of 12 to 20 mL/second should be used, depending on the size of the vein. Also, since contrast medium may remain in the arm vein for an extended period following injection, it may be advisable to flush the vein, immediately following injection with an appropriate volume (20 to 25 mL) of 5% Dextrose in water or normal saline.
15ARTERIAL DIGITAL SUBTRACTION ANGIOGRAPHY
Arterial digital subtraction angiography provides images similar in quality to conventional film-screen systems. The advantages of arterial DSA when compared to standard film angiography include: the use of less contrast medium; the use of lower concentrations for some procedures; a decreased need for selective arterial catheterization reducing the possibility of dislodging atheromatous plaques or significantly reducing the blood flow in the artery; and a shortened examination time. The limitations of arterial DSA include: reduced spatial resolution; limited field size; and the inability to conduct simultaneous biplane examinations.
15.1Patient Preparation
No special patient preparation is required for arterial DSA. However, it is advisable to ensure that patients are well hydrated prior to examination.
15.2Precautions
In addition to the general precautions described, the risks associated with arterial DSA are those usually attendant with catheter procedures. Following the procedure, gentle pressure hemostasis is required, followed by observation and immobilization of the limb for several hours to prevent hemorrhage from the site of arterial puncture.
15.3Usual Dosage
The following dosage schedule for adults should serve only as a guide since the volume administered, the concentration selected and the flow rate will be determined by the resolution of the equipment being used. As a general rule, the volume used and the flow rates for arterial DSA are 50% or less than that used for conventional film arteriography. Diagnostic studies have been obtained using Conray undiluted (28.2% iodine), diluted 1:1 (14.1% iodine), and diluted 1:2 (9.4% iodine). Sodium Chloride Injection USP or Water for Injection USP may be used for dilution.
The following doses, equivalent in iodine content to undiluted Conray, have been used.
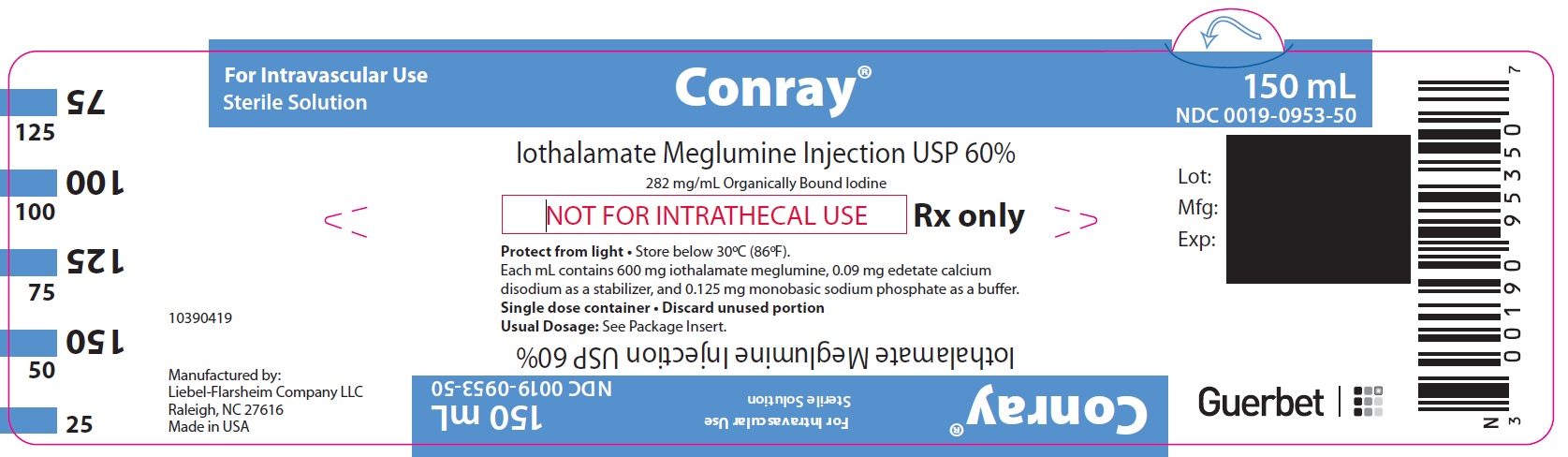
16Package Label Principal Display Panel - 150mL Bottle
For Intravascular Use
Sterile Solution
Sterile Solution
Conray
150mL
NDC 0019-0953-50
NDC 0019-0953-50
Iothalamate Meglumine Injection USP 60%
282 mg/mL Organically Bound Iodine
282 mg/mL Organically Bound Iodine
NOT FOR INTRATHECAL USE
Protect from light • Store below 30°C (86°F).
Each mL contains 600 mg iothalamate meglumine, 0.09 mg edetate calcium disodium as a stabilizer, and 0.125 mg monobasic sodium phosphate as a buffer.
Single dose container • Discard unused portion See Package Insert.
Each mL contains 600 mg iothalamate meglumine, 0.09 mg edetate calcium disodium as a stabilizer, and 0.125 mg monobasic sodium phosphate as a buffer.
Single dose container • Discard unused portion See Package Insert.
10390419
Manufactured by: