Brand Name
Terconazole
View Brand InformationFDA approval date: April 06, 2004
Classification: Azole Antifungal
Form: Suppository, Cream
What is Terconazole?
Terconazole Vaginal Suppositories, 80 mg is indicated for the local treatment of vulvovaginal candidiasis . As this product is effective only for vulvovaginitis caused by the genus Candida, the diagnosis should be confirmed by KOH smears and/or cultures.
Approved To Treat
Top Global Experts
There are no experts for this drug
Save this treatment for later
Not sure about your diagnosis?
Related Clinical Trials
There is no clinical trials being done for this treatment
Related Latest Advances
There is no latest advances for this treatment
Brand Information
Terconazole (Terconazole)
1DESCRIPTION
Terconazole Vaginal Cream 0.8% is a white to off-white, water washable cream for intravaginal administration containing 0.8% of the antifungal agent terconazole,
The structural formula of terconazole is as follows:
Terconazole, a triazole derivative, is a white to almost white powder with a molecular weight of 532.47. It is insoluble in water; sparingly soluble in ethanol; and soluble in butanol.
2INDICATIONS AND USAGE
Terconazole vaginal cream is indicated for the local treatment of vulvovaginal candidiasis (moniliasis). As terconazole vaginal cream is effective only for vulvovaginitis caused by the genus
3CONTRAINDICATIONS
Patients known to be hypersensitive to terconazole or to any of the components of the cream.
4WARNINGS
Anaphylaxis and toxic epidermal necrolysis have been reported during terconazole therapy. Terconazole therapy should be discontinued if anaphylaxis or toxic epidermal necrolysis develops.
5OVERDOSAGE
In the rat, the oral LD
In the event of oral ingestion of suppository or cream, supportive and symptomatic measures should be carried out. If the cream is accidentally applied to the eyes, wash with clean water or saline and seek medical attention if symptoms persist.
6DOSAGE AND ADMINISTRATION
One full applicator (5 grams) of terconazole vaginal cream (40 mg terconazole) should be administered intravaginally once daily at bedtime for three consecutive days.
Before prescribing another course of therapy, the diagnosis should be reconfirmed by smears and/or cultures and other pathogens commonly associated with vulvovaginitis ruled out. The therapeutic effect of terconazole vaginal cream is not affected by menstruation.
7HOW SUPPLIED
Terconazole Vaginal Cream 0.8% is available in 20 gram (NDC 51672-1302-0) tubes with 3 measured-dose applicators.
8Terconazole Vaginal Cream 0.8%
PATIENT INSTRUCTIONS
FILLING THE APPLICATOR:
- 1.Remove the cap from the tube.
- 2.Use the pointed tip on the top of the cap to puncture the seal on the tube.
- 3.Screw the applicator onto the tube.
- 4.Squeeze the tube from the bottom and fill the applicator until the plunger stops.
DO NOT release pressure on the tube until you have separated it from the filled applicator. - 5.Unscrew the applicator from the tube.
After each use, replace the cap and roll up the tube from the bottom.
USING THE APPLICATOR:
- 1.Lie on your back with your knees drawn up toward your chest.
- 2.Holding the applicator by the ribbed end of the barrel, insert the filled applicator into the vagina as far as it will comfortably go.
- 3.Slowly press the plunger of the applicator to release the cream into the vagina.
- 4.Remove the applicator from the vagina.
- 5.Apply one applicatorful each night for 3 nights at bedtime, as directed by your doctor.
Discard the applicator after each use.
NOTE:
A WORD ABOUT YEAST INFECTIONS
Why do yeast infections occur?
Yeast infections are caused by an organism called
How can I prevent yeast infections?
Certain factors may increase your chance of developing a yeast infection. These factors don't actually cause the problem, but they may create a situation that allows the yeast to grow rapidly.
- Clothing:Tight jeans, nylon underwear, pantyhose, and wet bathing suits can hold in heat and moisture (two conditions in which yeast organisms thrive). Looser pants or skirts, 100% cotton underwear, and stockings may help avoid this problem.
- Diet:Cutting down on sweets, milk products, and artificial sweeteners may reduce the risk of yeast infections.
- Antibiotics:Antibiotics work by eliminating disease-causing organisms. While they are helpful in curing other problems, antibiotics may lead to an overgrowth of Candidain the vagina.
- Pregnancy:Hormonal changes in the body during pregnancy encourage the growth of yeast. This is a very common time for an infection to occur. Until the baby is born, it may be hard to completely eliminate yeast infections. If you believe you are pregnant, tell your doctor.
- Menstruation:Sometimes monthly changes in hormone levels may lead to yeast infections.
- Diabetes:In addition to heat and moisture, yeast thrives on sugar. Because diabetics often have sugar in their urine, their vaginas are rich in this substance. Careful control of diabetes may help prevent yeast infection.
Controlling these factors can help eliminate yeast infections and may prevent them from coming back.
Some other helpful tips:
- 1.For best results, be sure to use the medication as prescribed by your doctor, even if you feel better quickly.
- 2.Avoid sexual intercourse, if your doctor advises you to do so.
- 3.If your partner has any penile itching, redness, or discomfort, he should consult his physician and mention that you are being treated for a yeast infection.
- 4.You can use the medication even if you are having your menstrual period. However, you should not use tampons because they may absorb the medication. Instead, use external pads or napkins until you have finished your medication. You may also wish to wear a sanitary napkin if the vaginal medication leaks.
- 5.Dry the genital area thoroughly after showering, bathing, or swimming. Change out of a wet bathing suit or damp exercise clothes as soon as possible. A dry environment is less likely to encourage the growth of yeast.
- 6.Wipe from front to rear (away from the vagina) after a bowel movement.
- 7.Don't douche unless your doctor specifically tells you to do so. Douching may disturb the vaginal balance.
- 8.Don't scratch if you can help it. Scratching can cause more irritation and spread the infection.
- 9.Discuss with your physician any medication you are already taking. Certain types of medication can make your vagina more susceptible to infection.
- 10.Eat nutritious meals to promote your general health.
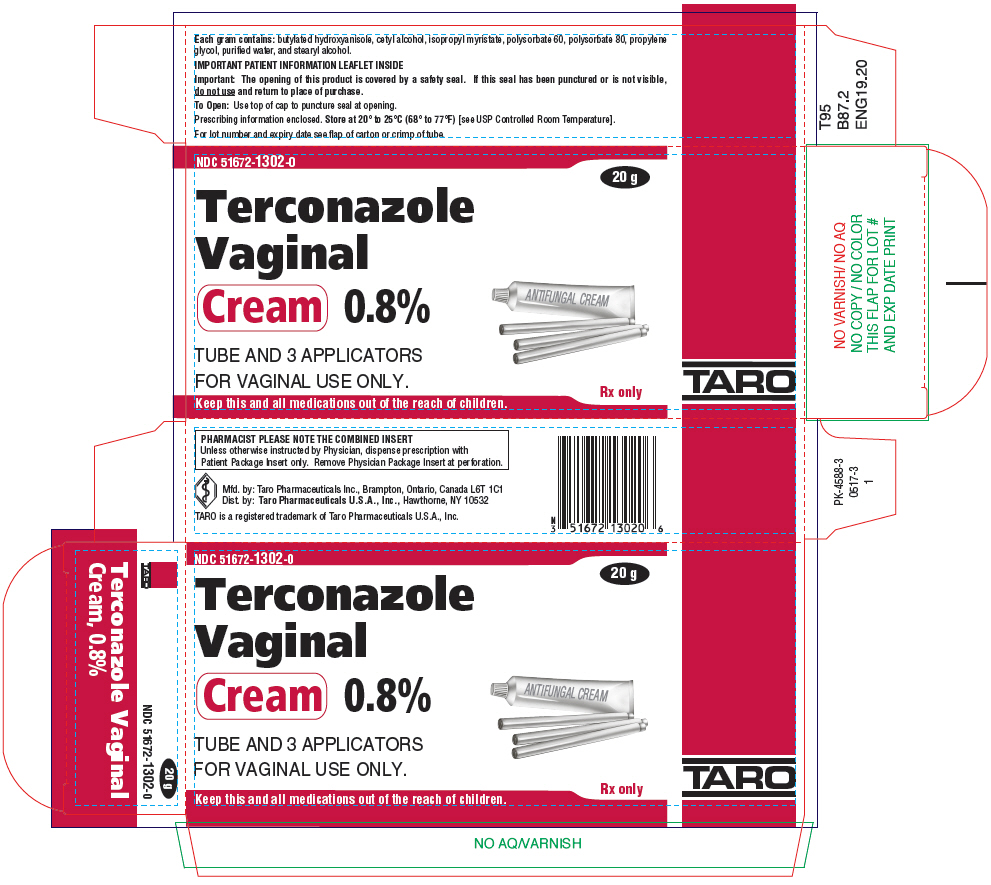
9PRINCIPAL DISPLAY PANEL - 20 g Tube Carton
NDC 51672-1302-0
20 g
Terconazole
TUBE AND 3 APPLICATORS
Rx only
Keep this and all medications out of the reach of children.
TARO