Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adult Safety Pools
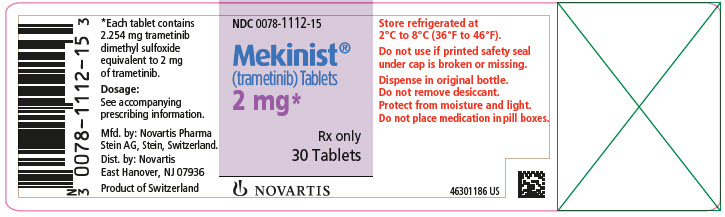
The pooled safety population described in the WARNINGS AND PRECAUTIONS reflects exposure to MEKINIST 2 mg orally, once daily as a single agent in 329 patients with various solid tumors enrolled in METRIC, MEK113583, and MEK111054. Among these 329 patients who received MEKINIST as a single agent, 33% were exposed for 6 months or longer and 9% were exposed for greater than one year.
The pooled safety population described in the WARNINGS AND PRECAUTIONS reflects exposure to MEKINIST 2 mg orally, once daily, administered in combination with dabrafenib 150 mg orally, twice daily, in 1087 patients enrolled in COMBI-d, COMBI-v, COMBI-AD, and BRF113928 with unresectable or metastatic melanoma, adjuvant melanoma, or NSCLC. Among these 1087 patients who received MEKINIST administered with dabrafenib, 70% were exposed for 6 months or longer and 21% were exposed for greater than one year.
Pediatric Safety Pool
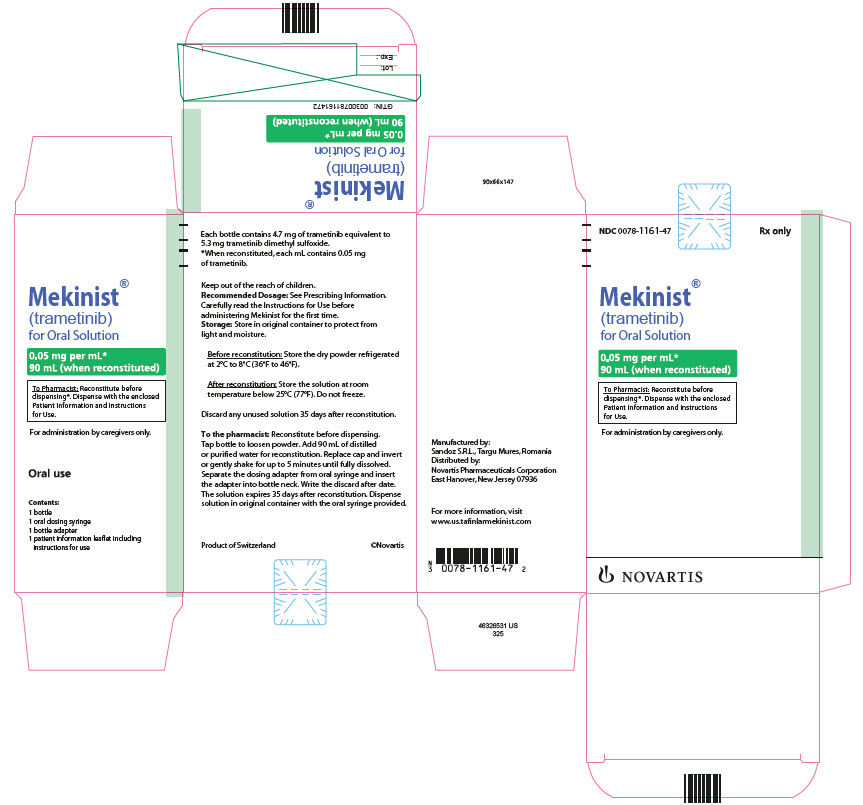
The pediatric pooled safety population described in the WARNINGS AND PRECAUTIONS reflects exposure to weight-based MEKINIST orally, once daily administered in combination with dabrafenib in 166 pediatric patients across two trials: a multi-center, open-label, multi-cohort study in pediatric patients with BRAF V600E mutation-positive glioma requiring systemic therapy (Study G2201; n = 123) and a multi-center, open-label, multi-cohort study in pediatric patients with refractory or recurrent solid tumors with MAPK pathway activation (Study X2101; n = 43)
Unresectable or Metastatic BRAF V600E or V600K Mutation-Positive Melanoma
MEKINIST as a Single Agent
The safety of MEKINIST was evaluated in the METRIC study, a randomized, open-label trial of patients with BRAF V600E or V600K mutation-positive unresectable or metastatic melanoma who received MEKINIST (N = 211) 2 mg orally once daily or chemotherapy (N = 99) (either dacarbazine 1000 mg/m
In this study, 9% of patients who received MEKINIST experienced adverse reactions resulting in permanent discontinuation of trial medication. The most frequent adverse reactions resulting in permanent discontinuation of MEKINIST were decreased LVEF, pneumonitis, renal failure, diarrhea, and rash. Adverse reactions led to dose reductions in 27% of patients treated with MEKINIST. Rash and decreased LVEF were the most frequent reasons cited for dose reductions of MEKINIST. Table 6 and Table 7 present adverse reactions and laboratory abnormalities, respectively, of MEKINIST as a single agent in the METRIC study.
Other clinically important adverse reactions for MEKINIST in a pool of MEKINIST monotherapy clinical studies observed in less than 10% of patients who received MEKINIST were:
Cardiac: Bradycardia, atrioventricular block, bundle branch block
Gastrointestinal: Dry mouth
Infections and Infestations: Folliculitis, rash pustular, cellulitis
Musculoskeletal and Connective Tissue: Rhabdomyolysis
Nervous System: Dizziness, dysgeusia, peripheral neuropathy
Ocular: Blurred vision, dry eye
MEKINIST with Dabrafenib
The safety of MEKINIST when administered with dabrafenib was evaluated in 559 patients with previously untreated, unresectable or metastatic, BRAF V600 mutation-positive melanoma who received MEKINIST in two trials, the COMBI-d study (n = 209), a multi-center, double-blind, randomized (1:1), active-controlled trial and the COMBI-v study (n = 350), a multi-center, open-label, randomized (1:1), active-controlled trial. In both trials, patients received MEKINIST 2 mg orally once daily and dabrafenib 150 mg orally twice daily until disease progression or unacceptable toxicity. Both trials excluded patients with abnormal LVEF, history of acute coronary syndrome within 6 months, history of Class II or greater congestive heart failure (New York Heart Association), history of RVO or RPED, QTcB interval ≥ 480 msec, uncontrolled hypertension, uncontrolled arrhythmias, active brain metastases, or known history of glucose-6-phosphate dehydrogenase deficiency
Among these 559 patients, 197 (35%) were exposed to MEKINIST for > 6 months to 12 months while 185 (33%) were exposed to MEKINIST for > 1 year. The median age was 55 years (range: 18 to 91), 57% were male, and 98% were White, 72% had baseline ECOG performance status of 0 and 28% had ECOG performance status of 1, 64% had M1c disease, 35% had elevated lactate dehydrogenase (LDH) at baseline, and 0.5% had a history of brain metastases.
The most common adverse reactions (≥ 20%) for MEKINIST in patients who received MEKINIST plus dabrafenib in the COMBI-d and COMBI-v studies were: pyrexia, nausea, rash, chills, diarrhea, vomiting, hypertension, and peripheral edema.
The demographics and baseline tumor characteristics of patients enrolled in the COMBI-d study are summarized in Clinical Studies
In the COMBI-d study, adverse reactions leading to discontinuation of MEKINIST occurred in 11% of patients who received MEKINIST plus dabrafenib; the most frequent were pyrexia (1.4%) and decreased ejection fraction (1.4%). Adverse reactions leading to dose reductions of MEKINIST occurred in 18% of patients who received MEKINIST plus dabrafenib; the most frequent were pyrexia (2.9%), neutropenia (1.9%), decreased ejection fraction (1.9%), and rash (1.9%). Adverse reactions leading to dose interruptions of MEKINIST occurred in 46% of patients who received MEKINIST plus dabrafenib; the most frequent were pyrexia (18%), chills (7%), vomiting (6%), and decreased ejection fraction (4.8%).
Table 8 and Table 9 present selected adverse reactions and laboratory abnormalities, respectively, of MEKINIST observed in the COMBI-d study.
Other clinically important adverse reactions for MEKINIST across the COMBI-d and COMBI-v studies (N = 559) observed in less than 10% of patients who received MEKINIST in combination with dabrafenib were:
Cardiac: Bradycardia, atrioventricular block, bundle branch block
Immune System: Sarcoidosis
Musculoskeletal and Connective Tissue: Rhabdomyolysis
Nervous System: Peripheral neuropathy, Guillain-Barré syndrome
Skin and Subcutaneous Tissue: Photosensitivity
Adjuvant Treatment of BRAF V600E or V600K Mutation-Positive Melanoma
The safety of MEKINIST when administered with dabrafenib was evaluated in 435 patients with Stage III melanoma with BRAF V600E or V600K mutations following complete resection who received at least one dose of study therapy in the COMBI-AD study
Patients who received MEKINIST in combination with dabrafenib had a median duration of exposure of 11 months (range: 0 to 12) to MEKINIST. Among the 435 patients who received MEKINIST in combination with dabrafenib, 72% were exposed to MEKINIST for > 6 months. The median age of patients who received MEKINIST in combination with dabrafenib was 50 years (range: 18 to 89), 56% were male, 99% were White, 92% had baseline ECOG performance status of 0, and 8% had baseline ECOG performance status of 1.
The most common adverse reactions (≥ 20%) in patients who received MEKINIST in combination with dabrafenib were: pyrexia, fatigue, nausea, headache, rash, chills, diarrhea, vomiting, arthralgia, and myalgia.
Adverse reactions resulting in discontinuation and dose interruptions of MEKINIST occurred in 24% and 54% of patients, respectively; the most frequent for each were pyrexia and chills. Adverse reactions leading to dose reductions of MEKINIST occurred in 23% of patients; the most frequent were pyrexia and decreased ejection fraction.
Table 10 summarizes the adverse reactions that occurred in at least 20% of the patients who received MEKINIST in combination with dabrafenib.
Other clinically important adverse reactions for MEKINIST in the COMBI-AD study observed in less than 20% of patients who received MEKINIST in combination with dabrafenib were: blurred vision (6%), decreased ejection fraction (5%), peripheral neuropathy (2.5%), rhabdomyolysis (< 1%), atrioventricular block (< 1%), Guillain-Barré syndrome (< 1%), and sarcoidosis (< 1%).
The laboratory abnormalities are summarized in Table 11.
Trial COMBI-APlus (Pyrexia Management Study)
COMBI-APlus evaluated the impact of pyrexia-related outcomes of a revised pyrexia management algorithm in patients who received dabrafenib administered with trametinib in the adjuvant treatment of BRAF V600 mutation-positive melanoma after complete resection. The pyrexia management algorithm interrupted both dabrafenib and trametinib when patient’s temperature is ≥ 100.4°F.
Grade 3-4 pyrexia occurred in 4.3% of patients, hospitalizations due to pyrexia occurred in 5.1% of patients, pyrexia with complications (dehydration, hypotension, renal dysfunction, syncope, severe chills) occurred in 2.2% of patients, and treatment discontinuation due to pyrexia occurred in 2.5% of patients.
Metastatic, BRAF V600E Mutation-Positive Non-Small Cell Lung Cancer
The safety of MEKINIST when administered with dabrafenib was evaluated in 93 patients with previously untreated (n = 36) and previously treated (n = 57) metastatic BRAF V600E mutation-positive NSCLC in a multi-center, multi-cohort, non-randomized, open-label trial (Study BRF113928). Patients received MEKINIST 2 mg orally once daily and dabrafenib 150 mg orally twice daily until disease progression or unacceptable toxicity. The trial excluded patients with abnormal LVEF, history of acute coronary syndrome within 6 months, history of Class II or greater congestive heart failure (New York Heart Association), QTc interval ≥ 480 msec, treatment refractory hypertension, uncontrolled arrhythmias, active brain metastases, history of ILD or pneumonitis, or history or current RVO
Among these 93 patients, 53 (57%) were exposed to MEKINIST and dabrafenib for > 6 months and 27 (29%) were exposed to MEKINIST and dabrafenib for ≥ 1 year. The median age was 65 years (range: 41 to 91), 46% were male, 85% were White; 32% had baseline ECOG performance status of 0 and 61% had ECOG performance status of 1; 98% had non-squamous histology; and 12% were current smokers, 60% were former smokers, and 28% had never smoked.
The most common adverse reactions (≥ 20%) in these 93 patients were: pyrexia, fatigue, nausea, vomiting, diarrhea, dry skin, decreased appetite, edema, rash, chills, hemorrhage, cough, and dyspnea.
Adverse reactions leading to discontinuation of MEKINIST occurred in 19% of patients; the most frequent were pyrexia (2.2%), decreased ejection fraction (2.2%), and respiratory distress (2.2%). Adverse reactions leading to dose reductions of MEKINIST occurred in 30% of patients; the most frequent were pyrexia (5%), nausea (4.3%), vomiting (4.3%), diarrhea (3.2%), and neutropenia (3.2%). Adverse reactions leading to dose interruptions of MEKINIST occurred in 57% of patients; the most frequent were pyrexia (16%), vomiting (10%), neutropenia (8%), nausea (5%), and decreased ejection fraction (5%).
Table 12 and Table 13 present adverse reactions and laboratory abnormalities, respectively, of MEKINIST in combination with dabrafenib in Study BRF113928.
Other clinically important adverse reactions for MEKINIST in Study BRF113928 observed in less than 20% of patients who received MEKINIST administered with dabrafenib were:
Cardiac: Atrioventricular block
Nervous System: Peripheral neuropathy
Advanced BRAF V600E Mutation-Positive Tumors
Study BRF117019
The safety of MEKINIST when administered with dabrafenib was evaluated in a multi-cohort, multi-center, non-randomized, open-label study in adult patients with cancers with the BRAF V600E mutation (Study BRF117019). A total of 206 patients were enrolled in the trial, 36 of whom were enrolled in the ATC cohort, 105 were enrolled in specific solid tumor cohorts, and 65 in other malignancies
Among these 206 patients, 101 (49%) were exposed to MEKINIST for ≥ 1 year and 103 (50%) were exposed to dabrafenib for ≥ 1 year. The median age was 60 years (range: 18 to 89); 56% were male; 79% were White; and 34% had baseline ECOG performance status of 0 and 60% had ECOG performance status of 1.
Serious adverse reactions occurred in 45% of patients who received MEKINIST in combination with dabrafenib. Serious adverse reactions in > 5% of patients included pyrexia (11%) and pneumonia (6%). Fatal adverse reactions occurred in 3.9% of patients who received MEKINIST in combination with dabrafenib. Fatal adverse reactions that occurred in > 1% of patients included sepsis (1.9%).
Permanent treatment discontinuation due to an adverse reaction occurred in 13% of patients. Adverse reactions which resulted in permanent treatment discontinuation in > 1% of patients included nausea (1.5%).
Dosage interruptions due to an adverse reaction occurred in 55% of patients. Adverse reactions which required dosage interruption in > 5% of patients included pyrexia (22%), chills (9%), fatigue (6%), neutropenia (6%), and nausea (5%).
Dose reductions due to an adverse reaction occurred in 44% of patients. Adverse reactions which required dose reductions in > 5% of patients included pyrexia (18%), chills (8%), and fatigue (6%).
The most common (≥ 20%) adverse reactions, including laboratory abnormalities, are listed in Table 14 and Table 15.
Table 14 summarizes the adverse reactions in Study BRF117019.
Clinically relevant adverse reactions for MEKINIST in Study BRF117019 observed in less than 20% of patients who received MEKINIST in combination with dabrafenib were: peripheral neuropathy (9%), decreased ejection fraction (8%), atrioventricular block (2.9%), uveitis (1.9%), hypersensitivity (1.9%) and Guillain-Barré syndrome (< 1%).
Table 15 summarizes the laboratory abnormalities in Study BRF117019.
BRAF V600E Mutation-Positive Solid Tumors in Pediatric Patients
Study CTMT212X2101 (X2101)
The safety of MEKINIST when administered with dabrafenib was evaluated in Study X2101, a multi-center, open-label, multi-cohort study in pediatric patients (n = 48) with refractory or recurrent solid tumors activation
Serious adverse reactions occurred in 46% of patients who received MEKINIST in combination with dabrafenib. Serious adverse reactions in > 5% of patients included pyrexia (25%) and decreased ejection fraction (6%). Permanent treatment discontinuation due to an adverse reaction occurred in 21% of patients. Adverse reactions which resulted in permanent treatment discontinuation in > 3% of patients included increased ALT (6%), increased AST (4.2%) and decreased ejection fraction (4.2%). Dosage interruptions due to an adverse reaction occurred in 73% of patients. Adverse reactions which required dosage interruption in > 5% of patients included pyrexia (56%), vomiting (19%), neutropenia (13%), rash (13%), decreased ejection fraction (6%), and uveitis (6%). Dose reductions due to an adverse reaction occurred in 25% of patients. Adverse reactions which required dose reductions in > 5% of patients included pyrexia (13%).
The most common (≥ 20%) adverse reactions, including laboratory abnormalities, are listed in Table 16 and Table 17.
Table 16 summarizes the adverse reactions in Study X2101.
Clinically relevant adverse reactions for MEKINIST in Study X2101 observed in less than 20% of patients (N=48) who received MEKINIST in combination with dabrafenib were: atrioventricular block (2.1%).
Table 17 summarizes the laboratory abnormalities in Study X2101.
BRAF V600E Mutation-Positive Low-Grade Glioma in Pediatric Patients
Study CDRB436G2201 (G2201)
The safety of MEKINIST in combination with dabrafenib was evaluated in pediatric patients 1 to < 18 years of age in Study G2201. Patients with low-grade glioma (LGG) who required first systemic therapy were randomized (2:1) to MEKINIST plus dabrafenib (n = 73) or carboplatin plus vincristine (n = 33). Nine patients crossed over from the carboplatin plus vincristine arm to the MEKINIST and dabrafenib arm. Pediatric patients received weight-based MEKINIST orally once daily administered in combination with dabrafenib until disease progression or intolerable toxicity. Patients in the control arm received carboplatin and vincristine at doses of 175 mg/m
The median age of these patients was 10 years (range: 1 to 17); 60% female; 75% White, 7% Asian, 2.7% Black or African American, 4% other race, and 11% where race was unknown or not reported.
Serious adverse reactions occurred in 40% of these patients. Serious adverse reactions in > 3% of patients included pyrexia (14%) and vomiting (4%).
Permanent discontinuation of MEKINIST due to an adverse reaction occurred in 4% of patients. Adverse reactions which resulted in permanent discontinuation of MEKINIST included chills, fatigue, pyrexia, weight increased, and headache.
Dosage interruptions of MEKINIST due to an adverse reaction occurred in 70% of patients. Adverse reactions which required a dosage interruption in > 5% of patients included pyrexia (52%).
Dose reductions of MEKINIST due to an adverse reaction occurred in 12% of patients. Adverse reactions which required dose reductions in > 2% of patients included weight increased (2.7%).
The most common (≥ 15%) adverse reactions were pyrexia (68%), rash (51%), headache (47%), vomiting (34%), musculoskeletal pain (34%), fatigue (33%), diarrhea (29%), dry skin (26%), nausea (25%), hemorrhage (25%), abdominal pain (25%), dermatitis acneiform (22%), dizziness (15%), upper respiratory tract infection (15%), and weight increased (15%).
The most common (≥ 20%) laboratory abnormalities that worsened from baseline were leukopenia (59%), increased alkaline phosphatase (55%), anemia (46%), decreased neutrophils (44%), increased AST (37%), decreased magnesium (34%), increased magnesium (32%), decreased platelets (30%), increased ALT (29%), and increased lymphocytes (24%).
Table 18 summarizes the adverse reactions in Study G2201.
Table 19 summarizes the laboratory abnormalities in Study G2201.