ALemtuzumab
What is Lemtrada (ALemtuzumab)?
Living with multiple sclerosis (MS) can feel like your body is working against you fatigue, numbness, and loss of coordination can make everyday activities unpredictable. For many, finding a treatment that slows the disease’s progression and restores stability is life-changing. Lemtrada (alemtuzumab) is one such medication that offers hope to people with relapsing forms of MS who have not responded well to other treatments.
Lemtrada is a monoclonal antibody, a laboratory-made protein that targets specific cells in the immune system. It belongs to a class of drugs designed to modify the immune response, helping reduce the attacks on the nervous system that cause MS symptoms. While it’s not a first-line treatment, Lemtrada is an important option for patients with active, relapsing multiple sclerosis who have had inadequate results with at least two other disease-modifying therapies.
Approved by the U.S. Food and Drug Administration (FDA) in 2014, Lemtrada is a specialized therapy administered under close medical supervision. Its unique dosing schedule and long-lasting effects distinguish it from many other MS treatments, offering a chance for extended periods of disease control after just a few annual treatment cycles.
What does Lemtrada do?
Lemtrada is used to treat relapsing forms of multiple sclerosis (MS), including relapsing-remitting MS (RRMS), the most common type of the disease. MS occurs when the immune system mistakenly attacks the protective myelin sheath surrounding nerve fibers in the brain and spinal cord, leading to inflammation and nerve damage. This can cause a wide range of symptoms, from vision problems and fatigue to muscle weakness and cognitive difficulties.
Lemtrada helps by reducing the number of relapses (flare-ups) and slowing the progression of physical disability. In clinical studies, patients taking Lemtrada experienced significantly fewer relapses and improved or stabilized neurological function compared with those taking other MS therapies (NIH, 2024).
For many patients, the benefits extend beyond fewer relapses; they often report greater day-to-day stability, reduced fatigue, and better control of symptoms. Because Lemtrada’s effects can last for years after treatment, it offers the possibility of long-term disease management with fewer ongoing doses.
How does Lemtrada work?
Lemtrada’s active ingredient, alemtuzumab, works by targeting a specific protein on immune cells called CD52. This protein is found on the surface of certain white blood cells particularly T and B lymphocytes, which are involved in the abnormal immune attack that damages the nervous system in MS.
When alemtuzumab binds to CD52, it destroys these overactive immune cells, temporarily reducing their numbers in the bloodstream. Over time, the immune system rebuilds itself, but in a more balanced way, with fewer cells that trigger MS attacks. This process, sometimes called immune system “resetting” , is what allows Lemtrada to deliver long-lasting benefits after a short course of treatment.
Clinically, this mechanism matters because it helps prevent further damage to the brain and spinal cord, protecting nerve function and slowing disability progression. While the immune system is temporarily weakened, careful monitoring ensures patients remain safe throughout recovery.
Lemtrada side effects
Because Lemtrada significantly alters the immune system, side effects are possible and can range from mild to serious. Understanding these effects helps patients stay alert and safe during treatment.
Common side effects may include:
- Headache
- Rash or itching
- Nausea
- Fatigue or fever after infusion
- Infections such as urinary tract or respiratory infections
Serious side effects (less common):
- Infusion reactions, including difficulty breathing, chest pain, or dizziness during or shortly after the infusion
- Autoimmune conditions, such as thyroid disorders or low platelet counts (which may cause easy bruising or bleeding)
- Kidney problems
- Increased risk of certain infections, including viral or bacterial infections
Lemtrada patients need close monitoring during and after infusions due to increased risk of autoimmune reactions and infections, even years later. Doctors perform regular blood and urine tests for at least four years post-treatment (FDA, 2024).
Lemtrada is contraindicated for those with active infections, HIV, or severe immune suppression. Pregnant women or those planning pregnancy should discuss risks, as Lemtrada can harm an unborn baby.
Seek immediate medical help for shortness of breath, facial swelling, severe rash, unexplained bleeding, or signs of infection (fever, persistent sore throat).
Lemtrada dosage
Lemtrada is administered via IV infusion in a hospital or clinic under professional supervision. Treatment involves two main courses: an initial series over consecutive days, followed by a shorter round a year later. Additional courses may be given if symptoms or disease activity persist. Patients are pretreated with corticosteroids to minimize infusion reactions, and doctors monitor for infections, potentially prescribing antivirals.
Regular lab tests (complete blood counts, thyroid, and kidney function) detect early complications. Patients should attend follow-up appointments and report unusual symptoms. Older adults or those with significant heart or kidney disease may need extra monitoring, but dosage adjustments are typically not required due to fixed Lemtrada infusion protocols.
Does Lemtrada have a generic version?
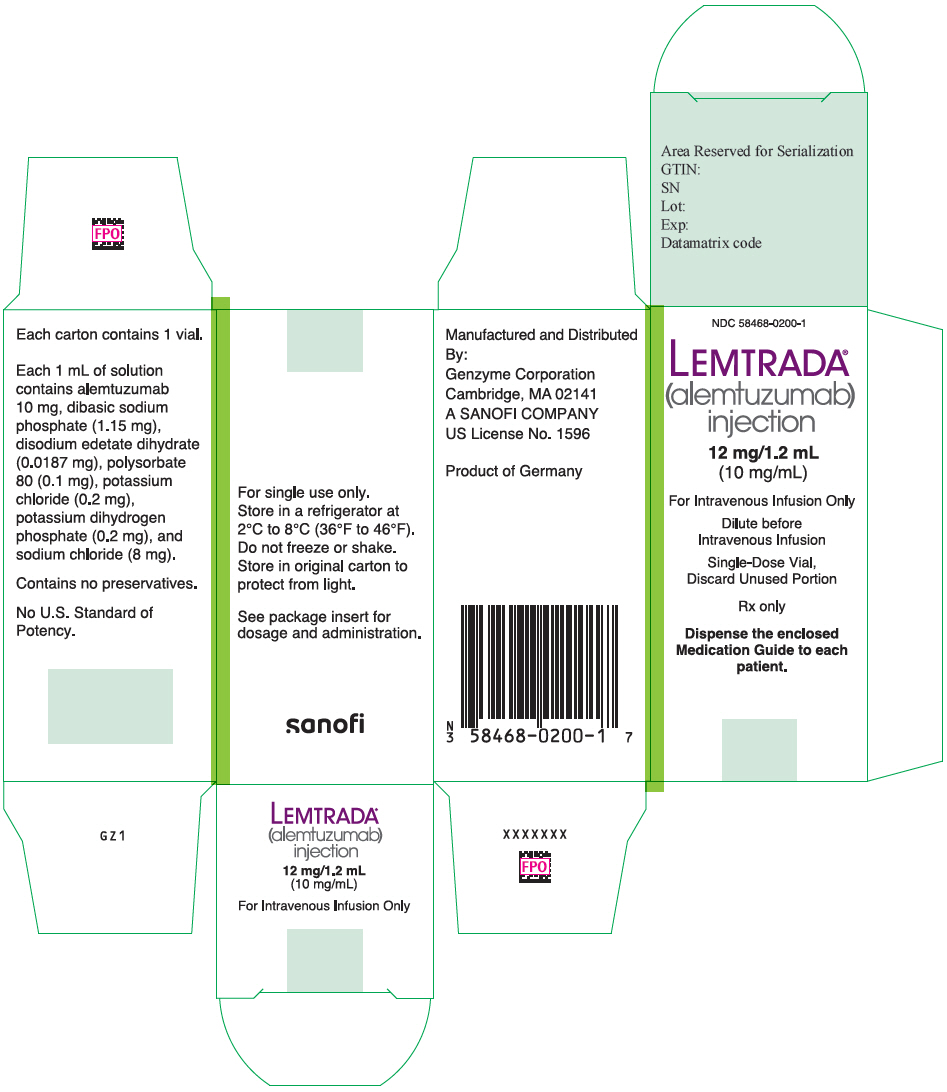
As of 2025, Lemtrada (alemtuzumab) does not have an FDA-approved generic version in the United States. It is only available under the brand name Lemtrada, manufactured by Sanofi Genzyme. However, international versions may exist in other markets.
Alemtuzumab (Campath) treats certain leukemias, but its oncology use differs significantly from its role in Lemtrada for other conditions. Dosing and monitoring vary, so never substitute without medical guidance. Future generic/biosimilar Lemtrada versions must meet FDA safety and effectiveness standards.
Conclusion
Lemtrada is a powerful disease-modifying therapy for people with relapsing forms of multiple sclerosis who have not found success with other treatments. By resetting the immune system, it helps reduce relapses, limit nerve damage, and slow the progression of disability often with long-lasting effects after only a few treatment cycles.
Despite significant risks, strict monitoring allows Lemtrada to offer strong protective effects for MS patients. Open communication with healthcare providers is essential, and when used responsibly, Lemtrada can greatly improve independence, energy, and quality of life for those with multiple sclerosis.
References
- U.S. Food and Drug Administration (FDA). (2024). Lemtrada (alemtuzumab) prescribing information. Retrieved from https://www.accessdata.fda.gov
- Mayo Clinic. (2024). Alemtuzumab (intravenous route) drug information. Retrieved from https://www.mayoclinic.org
- MedlinePlus. (2024). Alemtuzumab injection: Uses, side effects, and precautions. National Library of Medicine. Retrieved from https://medlineplus.gov
- National Institutes of Health (NIH). (2024). Disease-modifying therapies for multiple sclerosis. Retrieved from https://www.nih.gov
Approved To Treat
Related Clinical Trials
Summary: The purpose of this study is to determine whether a regimen of high-dose immunoablative therapy will demonstrate safety that is consistent or improved with other published regimens in SSc patients, while maintaining a treatment effect.
Summary: This is a multi-center prospective rater-masked (blinded) randomized controlled trial of 156 participants, comparing the treatment strategy of Autologous Hematopoietic Stem Cell Transplantation (AHSCT) to the treatment strategy of Best Available Therapy (BAT) for treatment-resistant relapsing multiple sclerosis (MS). Participants will be randomized at a 1 to 1 (1:1) ratio. All participants will be...
Summary: This multicenter prospective study seeks to determine if daratumumab given, prior to HLA-identical sibling donor transplantation using alemtuzumab, low dose total-body irradiation, and sirolimus, can prevent pure red blood cell aplasia with an acceptable safety profile in patients with anti-donor red blood cell antibodies, achieving an event-free survival similar to transplanted patients without s...
Related Latest Advances
Brand Information
- LEMTRADA causes serious, sometimes fatal, autoimmune conditions such as immune thrombocytopenia and anti-glomerular basement membrane disease. Monitor complete blood counts with differential, serum creatinine levels, and urinalysis with urine cell counts before starting treatment and then at monthly intervals until 48 months after the last dose of LEMTRADA
- LEMTRADA causes serious and life-threatening infusion reactions. LEMTRADA must be administered in a setting with appropriate equipment and personnel to manage anaphylaxis or serious infusion reactions. Monitor patients for two hours after each infusion. Make patients aware that serious infusion reactions can also occur after the 2-hour monitoring period
- Serious and life-threatening stroke (including ischemic and hemorrhagic stroke) has been reported within 3 days of LEMTRADA administration. Instruct patients to seek immediate medical attention if symptoms of stroke occur
- LEMTRADA may cause an increased risk of malignancies, including thyroid cancer, melanoma, and lymphoproliferative disorders. Perform baseline and yearly skin exams
- Because of the risk of autoimmunity, infusion reactions, and malignancies, LEMTRADA is available only through restricted distribution under a Risk Evaluation Mitigation Strategy (REMS) Program. Call 1-855-676-6326 to enroll in the LEMTRADA REMS program
- with known hypersensitivity or anaphylactic reactions to alemtuzumab or any of the excipients in LEMTRADA
- who are infected with human immunodeficiency virus (HIV) because LEMTRADA causes prolonged reductions of CD4+ lymphocyte counts
- with active infection
- Autoimmunity
- Infusion Reactions
- Stroke and Cervicocephalic Arterial Dissection
- Malignancies
- Immune Thrombocytopenia
- Glomerular Nephropathies Including Anti-glomerular Basement Membrane Disease
- Thyroid Disorders
- Other Autoimmune Cytopenias
- Autoimmune Hepatitis
- Hemophagocytic Lymphohistiocytosis
- Adult Onset Still's Disease
- Thrombotic Thrombocytopenic Purpura (TTP)
- Autoimmune Encephalitis (AIE)
- Acquired Hemophilia A
- Immune-Mediated Colitis
- Infections
- Progressive Multifocal Leukoencephalopathy (PML)
- Acute Acalculous Cholecystitis
- Pneumonitis