Generic Name
Deferasirox
Brand Names
Exjade, Jadenu, Deferasorox
FDA approval date: November 30, 2005
Classification: Iron Chelator
Form: Tablet, Granule
What is Exjade (Deferasirox)?
Deferasirox granule is an iron chelator indicated for the treatment of chronic iron overload due to blood transfusions in patients 2 years of age and older.
Top Global Experts
There are no experts for this drug
Save this treatment for later
Not sure about your diagnosis?
Related Clinical Trials
There is no clinical trials being done for this treatment
Related Latest Advances
There is no latest advances for this treatment
Brand Information
Exjade (deferasirox)
WARNING: RENAL FAILURE, HEPATIC FAILURE, and GASTROINTESTINAL HEMORRHAGE
Renal Failure
- Exjade can cause acute renal failure and death, particularly in patients with comorbidities and those who are in the advanced stages of their hematologic disorders.
- Evaluate baseline renal function prior to starting or increasing Exjade dosing in all patients. Exjade is contraindicated in adult and pediatric patients with eGFR less than 40 mL/min/1.73 m
Hepatic Failure
- Exjade can cause hepatic injury including hepatic failure and death.
- Measure serum transaminases and bilirubin in all patients prior to initiating treatment, every 2 weeks during the first month, and at least monthly thereafter.
- Avoid use of Exjade in patients with severe (Child-Pugh C) hepatic impairment and reduce the dose in patients with moderate (Child-Pugh B) hepatic impairment
Gastrointestinal Hemorrhage
- Exjade can cause gastrointestinal (GI) hemorrhages, which may be fatal, especially in elderly patients who have advanced hematologic malignancies and/or low platelet counts.
- Monitor patients and discontinue Exjade for suspected GI ulceration or hemorrhage
1DOSAGE FORMS AND STRENGTHS
- 125 mg tablets
- 250 mg tablets
- 500 mg tablets
2CONTRAINDICATIONS
Exjade is contraindicated in patients with:
- Estimated GFR less than 40 mL/min/1.73 m
- Poor performance status;
- High-risk myelodysplastic syndromes;
- Advanced malignancies.
- Platelet counts less than 50 x 10
- Known hypersensitivity to deferasirox or any component of Exjade
3ADVERSE REACTIONS
The following clinically significant adverse reactions are also discussed in other sections of the labeling:
- Acute Kidney Injury, Including Acute Renal Failure Requiring Dialysis, and Renal Tubular Toxicity Including Fanconi Syndrome
- Hepatic Toxicity and Failure
- GI Hemorrhage
- Bone Marrow Suppression
- Hypersensitivity
- Severe Skin Reactions
- Skin Rash
- Auditory and Ocular Abnormalities
3.1Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Transfusional Iron Overload
A total of 700 adult and pediatric patients were treated with Exjade (deferasirox) for 48 weeks in premarketing studies. These included 469 patients with beta-thalassemia, 99 with rare anemias, and 132 with sickle cell disease. Of these patients, 45% were male, 70% were Caucasian, and 292 patients were less than 16 years of age. In the sickle cell disease population, 89% of patients were black. Median treatment duration among the sickle cell patients was 51 weeks. Of the 700 patients treated, 469 (403 beta-thalassemia and 66 rare anemias) were entered into extensions of the original clinical protocols. In ongoing extension studies, median durations of treatment were 88-205 weeks.
Six hundred twenty-seven (627) patients with myelodysplastic syndrome (MDS) were enrolled across 5 uncontrolled trials. These studies varied in duration from 1 to 5 years. The discontinuation rate across studies in the first year was 46% (adverse events 20%, withdrawal of consent 10%, death 8%, other 4%, lab abnormalities 3%, and lack of efficacy 1%). Among 47 patients enrolled in the study of 5-year duration, 10 remained on Exjade at the completion of the study.
Table 1 displays adverse reactions occurring in greater than 5% of Exjade-treated beta-thalassemia patients (Study 1), sickle cell disease patients (Study 3), and patients with MDS (MDS pool). Abdominal pain, nausea, vomiting, diarrhea, skin rashes, and increases in serum creatinine were the most frequent adverse reactions reported with a suspected relationship to Exjade. Gastrointestinal symptoms, increases in serum creatinine, and skin rash were dose related.
In Study 1, a total of 113 (38%) patients treated with Exjade had increases in serum creatinine greater than 33% above baseline on 2 separate occasions (Table 2) and 25 (8%) patients required dose reductions. Increases in serum creatinine appeared to be dose related [see Warnings and Precautions (5.1)]. In this study, 17 (6%) patients treated with Exjade developed elevations in serum glutamic-pyruvic transaminase (SGPT)/ALT levels greater than 5 times the upper limit of normal (ULN) at 2 consecutive visits. Of these, 2 patients had liver biopsy proven drug-induced hepatitis and both discontinued Exjade therapy
In Study 3, a total of 48 (36%) patients treated with Exjade had increases in serum creatinine greater than 33% above baseline on 2 separate occasions (Table 2) [
In the MDS pool, in the first year, a total of 229 (37%) patients treated with Exjade had increases in serum creatinine greater than 33% above baseline on 2 consecutive occasions (Table 2) and 8 (3.5%) patients permanently discontinued
Non-Transfusion-Dependent Thalassemia Syndromes
In Study 5, 110 patients with NTDT received 1 year of treatment with Exjade 5 or 10 mg/kg/day and 56 patients received placebo in a double-blind, randomized trial. In Study 6, 130 of the patients who completed Study 5 were treated with open-label Exjade at 5, 10, or 20 mg/kg/day (depending on the baseline LIC) for 1 year
In Study 5, 1 patient in the placebo 10 mg/kg/day group experienced an ALT increase to greater than 5 times ULN and greater than 2 times baseline (Table 4). Three Exjade-treated patients (all in the 10 mg/kg/day group) had 2 consecutive serum creatinine level increases greater than 33% from baseline and greater than ULN. Serum creatinine returned to normal in all 3 patients (in 1 spontaneously and in the other 2 after drug interruption). Two additional cases of ALT increase and 2 additional cases of serum creatinine increase were observed in the 1-year extension of Study 5. The number (%) of patients with NTDT with increase in serum creatinine or SGPT/ALT in Study 5, Study 6, and Study 7 are presented in Table 4 below.
Proteinuria
In clinical studies, urine protein was measured monthly. Intermittent proteinuria (urine protein/creatinine ratio greater than 0.6 mg/mg) occurred in 18.6% of Exjade-treated patients compared to 7.2% of deferoxamine-treated patients in Study 1
Other Adverse Reactions
In the population of more than 5,000 patients with transfusional iron overload who have been treated with Exjade during clinical trials, adverse reactions occurring in 0.1% to 1% of patients included gastritis, edema, sleep disorder, pigmentation disorder, dizziness, anxiety, maculopathy, cholelithiasis, pyrexia, fatigue, laryngeal pain, cataract, hearing loss, GI hemorrhage, gastric ulcer (including multiple ulcers), duodenal ulcer, renal tubular disorder (Fanconi Syndrome), and acute pancreatitis (with and without underlying biliary conditions). Adverse reactions occurring in 0.01% to 0.1% of patients included optic neuritis, esophagitis, erythema multiforme, and drug reaction with eosinophilia and systemic symptoms (DRESS). Adverse reactions, which most frequently led to dose interruption or dose adjustment during clinical trials were rash, GI disorders, infections, increased serum creatinine, and increased serum transaminases.
Pooled Analysis of Pediatric Clinical Trial Data
A nested case control analysis was conducted within a deferasirox tablets for oral suspension pediatric pooled clinical trial dataset to evaluate the effects of dose and serum ferritin level, separately and combined, on kidney function. Among 1213 children (aged 2 to 15 years) with transfusion-dependent thalassemia, 162 cases of acute kidney injury (eGFR < 90 mL/min/1.73 m
- A 26% increased risk of acute kidney injury was observed with each 5 mg/kg increase in daily Exjade dosage starting at 20 mg/kg/day (95% confidence interval (CI): 1.08-1.48).
- A 25% increased risk for acute kidney injury was observed with each 250 mcg/L decrease in serum ferritin starting at 1250 mcg/L (95% CI: 1.01-1.56).
- Among pediatric patients with a serum ferritin < 1,000 mcg/L, those who received Exjade dosage > 30 mg/kg/day, compared to those who received lower dosages, had a higher risk for acute kidney injury (Odds ratio (OR) = 4.47, 95% CI: 1.25-15.95), consistent with overchelation.
In addition, a cohort based analysis of ARs was conducted in the deferasirox tablets for oral suspension pediatric pooled clinical trial data. Pediatric patients who received Exjade dose > 25 mg/kg/day when their serum ferritin was < 1,000 mcg/L (n = 158) had a 6-fold greater rate of renal adverse reactions (incidence rate ration (IRR) = 6.00, 95% CI: 1.75-21.36) and a 2-fold greater rate of dose interruptions (IRR = 2.06, 95% CI: 1.33-3.17) compared to the time-period prior to meeting these simultaneous criteria. Adverse reaction of special interest (cytopenia, renal, hearing, and GI disorders) occurred 1.9-fold more frequently when these simultaneous criteria were met, compared to preceding time-periods (IRR = 1.91, 95% CI: 1.05-3.48)
3.2Postmarketing Experience
The following adverse reactions have been spontaneously reported during postapproval use of Exjade in the transfusional-iron overload setting. Because these reactions are reported voluntarily from a population of uncertain size, in which patients may have received concomitant medication, it is not always possible to reliably estimate frequency or establish a causal relationship to drug exposure.
Skin and Subcutaneous Tissue Disorders: Stevens-Johnson syndrome (SJS), hypersensitivity vasculitis, urticaria, alopecia, toxic epidermal necrolysis (TEN)
Immune System Disorders: hypersensitivity reactions (including anaphylactic reaction and angioedema)
Renal and Urinary Disorders: acute renal failure, tubulointerstitial nephritis
Hepatobiliary Disorders: hepatic failure
Gastrointestinal Disorders: GI perforation
Blood and Lymphatic System Disorders: worsening anemia
5-Year Pediatric Registry
In a 5-year observational study, 267 pediatric patients 2 to < 6 years of age (at enrollment) with transfusional hemosiderosis received deferasirox. Of the 242 patients who had pre- and post-baseline eGFR measurements, 116 (48%) patients had a decrease in eGFR of ≥ 33% observed at least once. Twenty-one (18%) of these 116 patients with decreased eGFR had a dose interruption, and 15 (13%) of these 116 patients had a dose decrease within 30 days. Adverse reactions leading to permanent discontinuation from the study included liver injury (n = 11), renal tubular disorder
4OVERDOSAGE
Cases of overdose (2-3 times the prescribed dose for several weeks) have been reported. In one case, this resulted in hepatitis, which resolved without long-term consequences after a dose interruption. In one pediatric case, a dose of 2-3 times the prescribed dose for 6 days, resulted in acute renal failure requiring hemofiltration and acute liver injury/failure, which were reversible with intensive care support. Single doses up to 80 mg per kg per day in iron overloaded beta-thalassemic patients have been tolerated with nausea and diarrhea noted. In healthy volunteers, single doses of up to 40 mg per kg per day were tolerated.
Early signs of acute overdose are digestive effects such as abdominal pain, diarrhea, nausea, and vomiting. Hepatic and renal disorders have been reported, including cases of liver enzyme and creatinine increased with recovery after treatment discontinuation. An erroneously administered single dose of 90 mg/kg led to Fanconi syndrome which resolved after treatment.
There is no specific antidote for Exjade. In case of overdose, it may be treated with induction of vomiting or gastric lavage, and by symptomatic treatment.
5DESCRIPTION
Exjade (deferasirox) is an iron chelating agent. Exjade tablets for oral suspension contain 125 mg, 250 mg, or 500 mg deferasirox. Deferasirox is designated chemically as 4-[3,5-Bis (2-hydroxyphenyl)-1H-1,2,4-triazol-1-yl]-benzoic acid and its structural formula is:
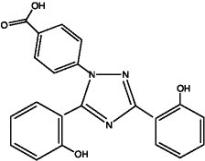
Deferasirox is a white to slightly yellow powder. Its molecular formula is C
Inactive Ingredients: Crospovidone (NF), lactose monohydrate (NF), magnesium stearate (NF), microcrystalline cellulose (NF), povidone (K30) (NF), silicon dioxide (NF), and sodium lauryl sulphate (NF).
6CLINICAL STUDIES
Transfusional Iron Overload
The primary efficacy study, Study 1 (NCT00061750), was a multicenter, open-label, randomized, active-comparator control study to compare Exjade (deferasirox) and deferoxamine in patients with beta-thalassemia and transfusional hemosiderosis. Patients greater than or equal to 2 years of age were randomized in a 1:1 ratio to receive either oral Exjade at starting doses of 5, 10, 20, or 30 mg per kg once daily or subcutaneous deferoxamine at starting doses of 20 to 60 mg per kg for at least 5 days per week based on LIC at baseline (2-3, greater than 3-7, greater than 7-14, and greater than 14 mg Fe/g dry weight). Patients randomized to deferoxamine who had LIC values less than 7 mg Fe/g dry weight were permitted to continue on their prior deferoxamine dose, even though the dose may have been higher than specified in the protocol.
Patients were to have a liver biopsy at baseline and end of study (after 12 months) for LIC. The primary efficacy endpoint was defined as a reduction in LIC of greater than or equal to 3 mg Fe/g dry weight for baseline values greater than or equal to 10 mg Fe/g dry weight, reduction of baseline values between 7 and less than 10 to less than 7 mg Fe/g dry weight, or maintenance or reduction for baseline values less than 7 mg Fe/g dry weight.
A total of 586 patients were randomized and treated, 296 with Exjade and 290 with deferoxamine. The mean age was 17.1 years (range, 2-53 years); 52% were females and 88% were Caucasian. The primary efficacy population consisted of 553 patients (Exjade n = 276; deferoxamine n = 277) who had LIC evaluated at baseline and 12 months or discontinued due to an adverse reaction. The percentage of patients achieving the primary endpoint was 52.9% for Exjade and 66.4% for deferoxamine. The relative efficacy of Exjade to deferoxamine cannot be determined from this study.
In patients who had an LIC at baseline and at end of study, the mean change in LIC was -2.4 mg Fe/g dry weight in patients treated with Exjade and -2.9 mg Fe/g dry weight in patients treated with deferoxamine.
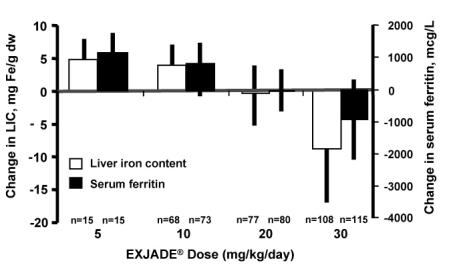
Reduction of LIC and serum ferritin was observed with Exjade doses of 20 to 30 mg per kg per day. Exjade doses below 20 mg per kg per day failed to provide consistent lowering of LIC and serum ferritin levels (Figure 1). Therefore, a starting dose of 20 mg per kg per day is recommended [
Study 2 (NCT00061763) was an open-label, noncomparative trial of efficacy and safety of Exjade given for 1 year to patients with chronic anemias and transfusional hemosiderosis. Similar to Study 1, patients received 5, 10, 20, or 30 mg per kg per day of Exjade based on baseline LIC.
A total of 184 patients were treated in this study: 85 patients with beta-thalassemia and 99 patients with other congenital or acquired anemias (myelodysplastic syndromes, n = 47; Diamond-Blackfan syndrome, n = 30; other, n = 22). Nineteen percent (19%) of patients were less than 16 years of age and 16% were greater than 65 years of age. There was a reduction in the absolute LIC from baseline to end of study (-4.2 mg Fe/g dry weight).
Study 3 (NCT00067080) was a multicenter, open-label, randomized trial of the safety and efficacy of Exjade relative to deferoxamine given for 1 year in patients with sickle cell disease and transfusional hemosiderosis. Patients were randomized to Exjade at doses of 5, 10, 20, or 30 mg per kg per day or subcutaneous deferoxamine at doses of 20-60 mg per kg per day for 5 days per week according to baseline LIC.
A total of 195 patients were treated in this study: 132 with Exjade and 63 with deferoxamine. Forty-four percent (44%) of patients were less than 16 years of age and 91% were black. At end of study, the mean change in LIC (as measured by magnetic susceptometry by a superconducting quantum interference device) in the per protocol-1 (PP-1) population, which consisted of patients who had at least 1 post-baseline LIC assessment, was -1.3 mg Fe/g dry weight for patients receiving Exjade (n = 113) and -0.7 mg Fe/g dry weight for patients receiving deferoxamine (n = 54).
One-hundred five (105) patients with thalassemia major and cardiac iron overload were enrolled in a study assessing the change in cardiac magnetic resonance imaging (MRI) T2* value (measured in milliseconds, ms) before and after treatment with deferasirox. Cardiac T2* values at baseline ranged from 5 to less than 20 ms. The geometric mean of cardiac T2* in the 68 patients who completed 3 years of Exjade therapy increased from 11.98 ms at baseline to 17.12 ms at 3 years. Cardiac T2* values improved in patients with severe cardiac iron overload (less than 10 ms) and in those with mild to moderate cardiac iron overload (greater than or equal to 10 to less than 20 ms). The clinical significance of these observations is unknown.
Six hundred twenty-seven (627) patients with MDS were enrolled across 5 uncontrolled trials. Two hundred thirty-nine (239) of the 627 patients were enrolled in trials that limited enrollment to patients with IPSS Low or Intermediate 1 risk MDS, and the remaining 388 patients were enrolled in trials that did not specify MDS risk stratification but required a life expectancy of greater than 1 year. Planned duration of treatment in these trials ranged from 1 year (365 patients) to 5 years (47 patients). These trials evaluated the effects of Exjade therapy on parameters of iron overload, including LIC (125 patients) and serum ferritin (627 patients). The percent of patients completing planned duration of treatment was 51% in the largest 1-year study, 52% in the 3-year study and 22% in the 5-year study. The major causes for treatment discontinuation were withdrawal of consent, adverse reaction, and death. Over 1 year of follow-up across these pooled studies, mean change in serum ferritin was -332.8 (± 2615.59) mcg/L (n = 593) and mean change in LIC was -5.9 (± 8.32) mg Fe/g dw (n = 68). Results of these pooled studies in 627 patients with MDS suggest a progressive decrease in serum ferritin and LIC beyond 1 year in those patients who are able to continue Exjade.
Study 4 (TELESTO; NCT00940602) was a randomized, double-blind, placebo-controlled trial performed in 225 patients with MDS (Low/Int-1 risk) and transfusional iron overload of which 149 were treated with deferasirox and 76 received placebo. The observed hazard ratio of 0.64 (95% CI: 0.42, 0.96) suggests a positive impact of deferasirox on event-free survival (EFS, a composite endpoint defined as death, worsening cardiac function, hospitalization for congestive heart failure, liver function impairment, liver cirrhosis, or progression to acute myeloid leukemia, whichever occurred first).
Non-Transfusion Dependent Thalassemia
Study 5 (NCT00873041) was a randomized, double-blind, placebo-controlled trial of treatment with Exjade for patients 10 years of age or older with NTDT syndromes and iron overload. Eligible patients had an LIC of at least 5 mg Fe/g dw measured by R2 MRI and a serum ferritin exceeding 300 mcg/L at screening (2 consecutive values at least 14 days apart from each other). A total of 166 patients were randomized, 55 to the Exjade 5 mg/kg/day dose group, 55 to the Exjade 10 mg/kg/day dose group, and 56 to placebo (28 to each matching placebo group). Doses could be increased after 6 months if the LIC exceeded 7 mg Fe/g dw and the LIC reduction from baseline was less than 15%. The patients enrolled included 89 males and 77 females. The underlying disease was beta-thalassemia intermedia in 95 (57%) patients, HbE beta-thalassemia in 49 (30%) patients, and alpha-thalassemia in 22 (13%) patients. There were 17 pediatric patients in the study. Caucasians comprised 57% of the study population and Asians comprised 42%. The median baseline LIC (range) for all patients was 12.1 (2.6-49.1) mg Fe/g dw. Follow-up was for 1 year. The primary efficacy endpoint of change in LIC from baseline to Week 52 was statistically significant in favor of both Exjade dose groups compared with placebo (p ≤ 0.001) (Table 5). Furthermore, a statistically significant dose effect of Exjade was observed in favor of the 10 mg/kg/day dose group (10 versus 5 mg/kg/day, p = 0.009). In a descriptive analysis, the target LIC (less than 5 mg Fe/g dw) was reached by 15 (27%) of 55 patients in the 10 mg/kg/day arm, 8 (15%) of 55 patients in the 5 mg/kg/day arm and 2 (4%) of 56 patients in the combined placebo groups.
Study 6 (NCT00873041) was an open-label trial of Exjade for the treatment of patients previously enrolled on Study 5, including cross-over to active treatment for those previously treated with placebo. The starting dose of Exjade in Study 6 was assigned based on the patient’s LIC at completion of Study 5, being 20 mg/kg/day for an LIC exceeding 15 mg Fe/g dw, 10 mg/kg/day for LIC 3-15 mg Fe/g dw, and observation if the LIC was less than 3 mg Fe/g dw. Patients could continue on 5 mg/kg/day if they had previously exhibited at least a 30% reduction in LIC. Doses could be increased to a maximum of 20 mg/kg/day after 6 months if the LIC was more than 7 mg Fe/g dw and the LIC reduction from baseline was less than 15%. The primary efficacy endpoint in Study 6 was the proportion of patients achieving an LIC less than 5 mg Fe/g dw. A total of 133 patients were enrolled. Twenty patients began Study 6 with an LIC less than 5 mg Fe/g dw. Of the 113 patients with a baseline LIC of at least 5 mg Fe/g dw in Study 6, the target LIC (less than 5 mg Fe/g dw) was reached by 39 patients (35%). The responders included 4 (10%) of 39 patients treated at 20 mg/kg/day for a baseline LIC exceeding 15 mg Fe/g dw, and 31 (51%) of 61 patients treated at 10 mg/kg/day for a baseline LIC between 5 and 15 mg Fe/g dw. The absolute change in LIC at Week 52 by starting dose is shown in Table 5 below.
Study 7 (NCT01709838) was an open-label, single-arm, multicenter, 5-year study to evaluate the efficacy and safety of Exjade in iron overloaded patients with NTDT of 10 years of age or older. All patients started treatment on 10 mg/kg/day Exjade for four weeks. At Week 4, dose escalation was based on baseline LIC. At Week 24 and every 6 months thereafter, further dose adjustments were made according to the LIC at that visit. Treatment was interrupted when LIC < 3 mg Fe/g dw or serum ferritin < 300 ng/mL and was restarted at 10 mg/kg/day when LIC ≥ 5 mg Fe/g dw and serum ferritin ≥ 300 ng/mL. Throughout the study, the maximum dose of Exjade given was 30 mg/kg/day.
A total of 134 patients were enrolled in the study. Eligible patients were required to have an LIC of at least 5 mg Fe/g dw measured by R2 MRI and a serum ferritin at least of 300 ng/mL at screening. The mean absolute change of LIC from Baseline to Week 52 was -6.7 mg Fe/g dw. The reduction in LIC was sustained until Week 260 (5 years) with the mean absolute change in LIC from Baseline to Week 260 of -10.6 mg Fe/g dw. In the subset of patients with Baseline LIC > 15 mg Fe/g dw (49 patients), 51.0% achieved a first LIC < 5 mg Fe/g dw (95% CI: 37.5, 64.4) with a median time of 28.6 months. In the subset of patients with target LIC of < 3 mg Fe/g dw (61 patients), 39.3% developed first LIC ≥ 5 mg Fe/g dw in the follow-up period, with a median time of 13.9 months.
7HOW SUPPLIED/STORAGE AND HANDLING
Exjade is provided as 125 mg, 250 mg, and 500 mg tablets for oral suspension.
125 mg
Off-white, round, flat tablet with beveled edge and imprinted with “J” and “125” on one side and “NVR” on the other.
Bottles of 30 tablets………………………………………………………………..(NDC 0078-0468-15)
250 mg
Off-white, round, flat tablet with beveled edge and imprinted with “J” and “250” on one side and “NVR” on the other.
Bottles of 30 tablets………………………………………………………………..(NDC 0078-0469-15)
500 mg
Off-white, round, flat tablet with beveled edge and imprinted with “J” and “500” on one side and “NVR” on the other.
Bottles of 30 tablets………………………………………………………………..(NDC 0078-0470-15)
Store Exjade tablets at 20°C to 25°C (68°F to 77°F); excursions are permitted between 15°C to 30°C (59°F to 86°F) [see USP Controlled Room Temperature]. Protect from moisture.
8PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Dosing Instructions
Advise patients to take Exjade once daily on an empty stomach at least 30 minutes prior to food, preferably at the same time every day. Instruct patients to completely disperse the tablets in water, orange juice, or apple juice, and drink the resulting suspension immediately. After the suspension has been swallowed, resuspend any residue in a small volume of the liquid and swallow
Advise patients not to chew tablets or swallow them whole
Blood Testing
Advise patients that blood tests will be performed frequently to check for damage to kidneys, liver, or blood cells
Acute Kidney Injury, Including Acute Renal Failure
Caution patients about the potential for kidney toxicity when taking Exjade. Inform patients of the signs and symptoms of kidney injury. Advise patients to contact their healthcare provider immediately if they experience any of these symptoms
Hepatic Toxicity and Failure
Caution patients about the potential for hepatic toxicity when taking Exjade. Inform patients of the signs and symptoms of hepatic toxicity. Advise patients to contact their healthcare provider immediately if they experience any of these symptoms
GI Ulceration and Hemorrhage
Caution patients about the potential for the development of GI ulcers or bleeding when taking Exjade in combination with drugs that have ulcerogenic or hemorrhagic potential, such as NSAIDs, corticosteroids, oral bisphosphonates, or anticoagulants. Inform patients of the signs and symptoms of GI ulcers or bleeding. Advise patients to contact their health care provider for symptoms of heartburn but to seek immediate medical attention for symptoms of GI hemorrhage
Allergic Reactions
Serious allergic reactions (which include swelling of the throat) have been reported in patients taking Exjade, usually within the first month of treatment. If reactions are severe, advise patients to stop taking Exjade immediately and seek immediate medical attention
Severe Skin Reactions
Severe skin reactions have been reported in patients taking Exjade. Inform patients of the signs and symptoms of severe skin reactions. If reactions are severe, advise patients to stop taking Exjade immediately and seek immediate medical attention
Skin Rash
Skin rashes may occur during Exjade treatment. If the skin rash is severe, advise patients to stop taking Exjade and seek medical attention
Pediatric Patients with Acute Illness
Instruct pediatric patients and their caregivers to contact their healthcare provider during episodes of acute illness, especially if the patient has not been drinking fluids or the patient has volume depletion due to fever, vomiting, or diarrhea
Auditory and Ocular Testing
Because auditory and ocular disturbances have been reported with Exjade, conduct auditory testing and ophthalmic testing before starting Exjade treatment and thereafter at regular intervals. Advise patients to contact their healthcare provider if they develop visual or auditory changes during treatment
Drug Interactions
Caution patients not to take aluminum-containing antacids and Exjade simultaneously
Caution patients about potential loss of effectiveness of drugs metabolized by CYP3A4 (e.g., cyclosporine, simvastatin, hormonal contraceptive agents) when Exjade is administered with these drugs
Caution patients about potential loss of effectiveness of Exjade when administered with drugs that are potent UGT inducers (e.g., rifampicin, phenytoin, phenobarbital, ritonavir). Based on serum ferritin levels and clinical response, consider increases in the dose of Exjade when concomitantly used with potent UGT inducers
Caution patients about potential loss of effectiveness of Exjade when administered with drugs that are bile acid sequestrants (e.g., cholestyramine, colesevelam, colestipol). Based on serum ferritin levels and clinical response, consider increases in the dose of Exjade when concomitantly used with bile acid sequestrants
Caution patients with diabetes to monitor their glucose levels more frequently when repaglinide is used concomitantly with Exjade
Driving and Using Machines
Caution patients experiencing dizziness to avoid driving or operating machinery
Distributed by:
© Novartis
T2020-105
9PRINCIPAL DISPLAY PANEL
NDC 0078-0468-15 Rx only
EXJADE
Tablets for Oral Suspension*
125 mg per tablet
PHARMACIST: Dispense with accompanying
DO NOT CHEW OR SWALLOW WHOLE
*Tablets MUST be dispersed in water,
orange or apple juice
NOVARTIS 30 Tablets
10PRINCIPAL DISPLAY PANEL
NDC 0078-0469-15 Rx only
EXJADE
Tablets for Oral Suspension*
250 mg per tablet
PHARMACIST: Dispense with accompanying
DO NOT CHEW OR SWALLOW WHOLE
*Tablets MUST be dispersed in water,
orange or apple juice
NOVARTIS 30 Tablets
11PRINCIPAL DISPLAY PANEL
NDC 0078-0470-15 Rx only
EXJADE
Tablets for Oral Suspension*
500 mg per tablet
PHARMACIST: Dispense with accompanying
DO NOT CHEW OR SWALLOW WHOLE
*Tablets MUST be dispersed in water,
orange or apple juice
NOVARTIS 30 Tablets
