Brand Name
Vfend
Generic Name
Voriconazole
View Brand Information FDA approval date: May 24, 2002
Classification: Azole Antifungal
Form: Injection, Tablet, Powder, Suspension
What is Vfend (Voriconazole)?
Voriconazole for Injection is an azole antifungal indicated for the treatment of adults and pediatric patients 2 years of age and older with: Invasive aspergillosis.
Approved To Treat
Top Global Experts
There are no experts for this drug
Save this treatment for later
Not sure about your diagnosis?
Related Clinical Trials
There is no clinical trials being done for this treatment
Related Latest Advances
There is no latest advances for this treatment
Brand Information
VFEND (VORICONAZOLE)
1CONTRAINDICATIONS
- VFEND is contraindicated in patients with known hypersensitivity to voriconazole or its excipients. There is no information regarding cross-sensitivity between VFEND (voriconazole) and other azole antifungal agents. Caution should be used when prescribing VFEND to patients with hypersensitivity to other azoles.
- Coadministration of pimozide, quinidine or ivabradine with VFEND is contraindicated because increased plasma concentrations of these drugs can lead to QT prolongation and rare occurrences of
- Coadministration of VFEND with sirolimus is contraindicated because VFEND significantly increases sirolimus concentrations
- Coadministration of VFEND with rifampin, carbamazepine, long-acting barbiturates or St. John's Wort is contraindicated because these drugs are likely to decrease plasma voriconazole concentrations significantly
- Coadministration of standard doses of voriconazole with efavirenz doses of 400 mg every 24 hours or higher is contraindicated, because efavirenz significantly decreases plasma voriconazole concentrations in healthy subjects at these doses. Voriconazole also significantly increases efavirenz plasma concentrations
- Coadministration of VFEND with high-dose ritonavir (400 mg every 12 hours) is contraindicated because ritonavir (400 mg every 12 hours) significantly decreases plasma voriconazole concentrations. Coadministration of voriconazole and low-dose ritonavir (100 mg every 12 hours) should be avoided, unless an assessment of the benefit/risk to the patient justifies the use of voriconazole
- Coadministration of VFEND with rifabutin is contraindicated since VFEND significantly increases rifabutin plasma concentrations and rifabutin also significantly decreases voriconazole plasma concentrations
- Coadministration of VFEND with ergot alkaloids (ergotamine and dihydroergotamine) is contraindicated because VFEND may increase the plasma concentration of ergot alkaloids, which may lead to ergotism
- Coadministration of VFEND with naloxegol is contraindicated because VFEND may increase plasma concentrations of naloxegol which may precipitate opioid withdrawal symptoms
- Coadministration of VFEND with tolvaptan is contraindicated because VFEND may increase tolvaptan plasma concentrations and increase risk of adverse reactions
- Coadministration of VFEND with venetoclax at initiation and during the ramp-up phase is contraindicated in patients with chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL) due to the potential for increased risk of tumor lysis syndrome
- Coadministration of VFEND with lurasidone is contraindicated since it may result in significant increases in lurasidone exposure and the potential for serious adverse reactions
- Coadministration of VFEND with finerenone is contraindicated since it may result in significant increases in finerenone exposure and the potential for serious adverse reactions
2ADVERSE REACTIONS
The following serious adverse reactions are described elsewhere in the labeling:
Hepatic Toxicity
Arrhythmias and QT Prolongation
Infusion Related Reactions
Visual Disturbances
Severe Cutaneous Adverse Reactions
Photosensitivity
Renal Toxicity
2.1Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
2.2Postmarketing Experience in Adult and Pediatric Patients
The following adverse reactions have been identified during post-approval use of VFEND. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Dermatological Reactions
Increased risk of skin toxicity with concomitant use of methotrexate, a drug associated with UV reactivation, was observed in postmarketing reports
3DRUG INTERACTIONS
Voriconazole is metabolized by cytochrome P450 isoenzymes, CYP2C19, CYP2C9, and CYP3A4. Therefore, inhibitors or inducers of these isoenzymes may increase or decrease voriconazole plasma concentrations, respectively. Voriconazole is a strong inhibitor of CYP3A4, and also inhibits CYP2C19 and CYP2C9. Therefore, voriconazole may increase the plasma concentrations of substances metabolized by these CYP450 isoenzymes.
Tables 10 and 11 provide the clinically significant interactions between voriconazole and other medical products.
4OVERDOSAGE
In clinical trials, there were three cases of accidental overdose. All occurred in pediatric patients who received up to five times the recommended intravenous dose of voriconazole. A single adverse reaction of photophobia of 10 minutes duration was reported.
There is no known antidote to voriconazole.
Voriconazole is hemodialyzed with clearance of 121 mL/min. The intravenous vehicle, SBECD, is hemodialyzed with clearance of 55 mL/min. In an overdose, hemodialysis may assist in the removal of voriconazole and SBECD from the body.
5DESCRIPTION
VFEND (voriconazole), an azole antifungal agent is available as a lyophilized powder for solution for intravenous infusion. The structural formula is:
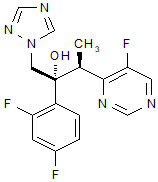
Voriconazole is designated chemically as (2R,3S)-2-(2, 4-difluorophenyl)-3-(5-fluoro-4-pyrimidinyl)-1-(1
Voriconazole drug substance is a white to light-colored powder.
VFEND I.V. is a white lyophilized powder containing nominally 200 mg voriconazole and 3200 mg sulfobutyl ether beta-cyclodextrin sodium in a 30 mL Type I clear glass vial.
VFEND I.V. is intended for administration by intravenous infusion. It is a single-dose, unpreserved product. Vials containing 200 mg lyophilized voriconazole are intended for reconstitution with Water for Injection to produce a solution containing 10 mg/mL VFEND and 160 mg/mL of sulfobutyl ether beta-cyclodextrin sodium. The resultant solution is further diluted prior to administration as an intravenous infusion
6CLINICAL STUDIES
Voriconazole, administered orally or parenterally, has been evaluated as primary or salvage therapy in 520 patients aged 12 years and older with infections caused by
6.1Invasive Aspergillosis (IA)
Voriconazole was studied in patients for primary therapy of IA (randomized, controlled study 307/602), for primary and salvage therapy of aspergillosis (non-comparative study 304) and for treatment of patients with IA who were refractory to, or intolerant of, other antifungal therapy (non-comparative study 309/604).
6.2Candidemia in Non-neutropenic Patients and Other Deep Tissue CandidaInfections
Voriconazole was compared to the regimen of amphotericin B followed by fluconazole in Study 608, an open-label, comparative study in nonneutropenic patients with candidemia associated with clinical signs of infection. Patients were randomized in 2:1 ratio to receive either voriconazole (n=283) or the regimen of amphotericin B followed by fluconazole (n=139). Patients were treated with randomized study drug for a median of 15 days. Most of the candidemia in patients evaluated for efficacy was caused by
An independent Data Review Committee (DRC), blinded to study treatment, reviewed the clinical and mycological data from this study, and generated one assessment of response for each patient. A successful response required all of the following: resolution or improvement in all clinical signs and symptoms of infection, blood cultures negative for
The overall clinical and mycological success rates by
In a secondary analysis, which counted DRC-assessed successes at any time point (EOT, or 2, 6, or 12 weeks after EOT), the response rates were 65% for voriconazole and 71% for the regimen of amphotericin B followed by fluconazole.
In Studies 608 and 309/604 (non-comparative study in patients with invasive fungal infections who were refractory to, or intolerant of, other antifungal agents), voriconazole was evaluated in 35 patients with deep tissue
6.3Esophageal Candidiasis (EC)
The efficacy of oral voriconazole 200 mg twice daily compared to oral fluconazole 200 mg once daily in the primary treatment of EC was demonstrated in Study 150-305, a double-blind, double-dummy study in immunocompromised patients with endoscopically-proven EC. Patients were treated for a median of 15 days (range 1 to 49 days). Outcome was assessed by repeat endoscopy at end of treatment (EOT). A successful response was defined as a normal endoscopy at EOT or at least a 1 grade improvement over baseline endoscopic score. For patients in the Intent-to-Treat (ITT) population with only a baseline endoscopy, a successful response was defined as symptomatic cure or improvement at EOT compared to baseline. Voriconazole and fluconazole (200 mg once daily) showed comparable efficacy rates against EC, as presented in Table 16.
Microbiologic success rates by
6.4Other Serious Fungal Pathogens
In pooled analyses of patients, voriconazole was shown to be effective against the following additional fungal pathogens:
6.5Pediatric Studies
A total of 22 patients aged 12 to 18 years with IA were included in the adult therapeutic studies. Twelve out of 22 (55%) patients had successful response after treatment with a maintenance dose of voriconazole 4 mg/kg every 12 hours.
Fifty-three pediatric patients aged 2 to less than 18 years old were treated with voriconazole in two prospective, open-label, non-comparative, multicenter clinical studies.
One study was designed to enroll pediatric patients with IA or infections with rare molds (such as
The study enrolled 31 patients with possible, proven, or probable IA. Fourteen of 31 patients, 5 of whom were 2 to less than 12 years old and 9 of whom were 12 to less than 18 years old, had proven or probable IA and were included in the modified intent-to-treat (MITT) efficacy analyses. No patients with rare mold were enrolled. A successful global response was defined as resolution or improvement in clinical signs and symptoms and at least 50% resolution of radiological lesions attributed to IA. The overall rate of successful global response at 6 weeks in the MITT population is presented in Table 18 below.
The second study enrolled 22 patients with invasive candidiasis including candidemia (ICC) and EC requiring either primary or salvage therapy. Patients with ICC aged 2 to less than 12 years and 12 to 14 years with body weight less than 50 kg received an intravenous VFEND loading dose of 9 mg/kg every 12 hours for the first 24 hours followed by an 8 mg/kg intravenous maintenance dose every 12-hours. After completing 5 days of intravenous therapy patients had an option to switch to oral VFEND. The oral maintenance dose was 9 mg/kg every 12 hours (maximum dose of 350 mg). All other pediatric patients aged 12 to less than 18 years received the adult VFEND dosage regimen. VFEND was administered for at least 14 days after the last positive culture. A maximum of 42 days of treatment was permitted.
Patients with primary or salvage EC aged 2 to less than 12 years and 12 to 14 years with body weight less than 50 kg received an intravenous VFEND dose of 4 mg/kg every 12 hours followed by an oral VFEND dose of 9 mg/kg every 12 hours (maximum dose of 350 mg) when criteria for oral switch were met. All other pediatric patients aged 12 to less than 18 years received the adult VFEND dosage regimen. VFEND was administered for at least 7 days after the resolution of clinical signs and symptoms. A maximum of 42 days of treatment was permitted.
For EC, study treatment was initiated without a loading dose of intravenous voriconazole. Seventeen of these patients had confirmed
7PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Visual Disturbances
Patients should be instructed that visual disturbances such as blurring and sensitivity to light may occur with the use of VFEND.
Photosensitivity
- Advise patients of the risk of photosensitivity (with or without concomitant methotrexate), accelerated photoaging, and skin cancer.
- Advise patients that VFEND can cause serious photosensitivity and to immediately contact their healthcare provider for new or worsening skin rash.
- Advise patients to avoid exposure to direct sun light and to use measures such as protective clothing and sunscreen with high sun protection factor (SPF).
Embryo-Fetal Toxicity
- Advise female patients of the potential risks to a fetus.
- Advise females of reproductive potential to use effective contraception during treatment with VFEND.
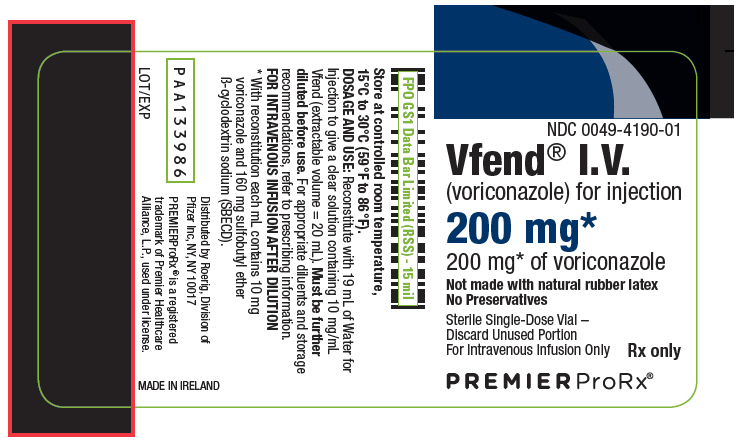
8PRINCIPAL DISPLAY PANEL - 200 mg Vial Label
NDC 0049-4190-01
Vfend
(voriconazole) for injection
(voriconazole) for injection
200 mg*
200 mg* of voriconazole
200 mg* of voriconazole
Not made with natural rubber latex
No Preservatives
No Preservatives
Sterile Single-Dose Vial –
Rx only
PREMIERProRx®
9PRINCIPAL DISPLAY PANEL - 200 mg Vial Carton
NDC 0049-4190-01
1 Vial
200 mg*
200 mg* of voriconazole
200 mg* of voriconazole
Not made with natural
rubber latex
No Preservatives
rubber latex
No Preservatives
Sterile Single-Dose Vial –
For Intravenous Infusion Only
PREMIERProRx®
