Generic Name
Carbamazepine
Brand Names
Carbatrol, Tegretol, Equetro, Epitol, Carbamazepin
FDA approval date: March 11, 1968
Classification: Mood Stabilizer
Form: Tablet, Suspension, Capsule
What is Carbatrol (Carbamazepine)?
Epilepsy Carbamazepine is indicated for use as an anticonvulsant drug. Evidence supporting efficacy of carbamazepine as an anticonvulsant was derived from active drug-controlled studies that enrolled patients with the following seizure types: Partial seizures with complex symptomatology . Patients with these seizures appear to show greater improvement than those with other types. Generalized tonic-clonic seizures . Mixed seizure patterns which include the above, or other partial or generalized seizures. Absence seizures do not appear to be controlled by carbamazepine. Trigeminal Neuralgia Carbamazepine is indicated in the treatment of the pain associated with true trigeminal neuralgia. Beneficial results have also been reported in glossopharyngeal neuralgia. This drug is not a simple analgesic and should not be used for the relief of trivial aches or pains.
Top Global Experts
There are no experts for this drug
Save this treatment for later
Not sure about your diagnosis?
Related Clinical Trials
There is no clinical trials being done for this treatment
Related Latest Advances
There is no latest advances for this treatment
Brand Information
Carbatrol (carbamazepine)
WARNING
SERIOUS DERMATOLOGIC REACTIONS AND HLA-B*1502 ALLELE
SERIOUS AND SOMETIMES FATAL DERMATOLOGIC REACTIONS, INCLUDING TOXIC EPIDERMAL NECROLYSIS (TEN) AND STEVENS-JOHNSON SYNDROME (SJS), HAVE BEEN REPORTED DURING TREATMENT WITH CARBAMAZEPINE. THESE REACTIONS ARE ESTIMATED TO OCCUR IN 1 TO 6 PER 10,000 NEW USERS IN COUNTRIES WITH MAINLY CAUCASIAN POPULATIONS, BUT THE RISK IN SOME ASIAN COUNTRIES IS ESTIMATED TO BE ABOUT 10 TIMES HIGHER. STUDIES IN PATIENTS OF CHINESE ANCESTRY HAVE FOUND A STRONG ASSOCIATION BETWEEN THE RISK OF DEVELOPING SJS/TEN AND THE PRESENCE OF HLA-B*1502, AN INHERITED ALLELIC VARIANT OF THE HLA-B GENE. HLA-B*1502 IS FOUND ALMOST EXCLUSIVELY IN PATIENTS WITH ANCESTRY ACROSS BROAD AREAS OF ASIA. PATIENTS WITH ANCESTRY IN GENETICALLY AT-RISK POPULATIONS SHOULD BE SCREENED FOR THE PRESENCE OF HLA-B*1502 PRIOR TO INITIATING TREATMENT WITH CARBATROL).
APLASTIC ANEMIA AND AGRANULOCYTOSIS
APLASTIC ANEMIA AND AGRANULOCYTOSIS HAVE BEEN REPORTED IN ASSOCIATION WITH THE USE OF CARBAMAZEPINE. DATA FROM A POPULATION-BASED CASE-CONTROL STUDY DEMONSTRATE THAT THE RISK OF DEVELOPING THESE REACTIONS IS 5-8 TIMES GREATER THAN IN THE GENERAL POPULATION. HOWEVER, THE OVERALL RISK OF THESE REACTIONS IN THE UNTREATED GENERAL POPULATION IS LOW, APPROXIMATELY SIX PATIENTS PER ONE MILLION POPULATION PER YEAR FOR AGRANULOCYTOSIS AND TWO PATIENTS PER ONE MILLION POPULATION PER YEAR FOR APLASTIC ANEMIA.
ALTHOUGH REPORTS OF TRANSIENT OR PERSISTENT DECREASED PLATELET OR WHITE BLOOD CELL COUNTS ARE NOT UNCOMMON IN ASSOCIATION WITH THE USE OF CARBAMAZEPINE, DATA ARE NOT AVAILABLE TO ESTIMATE ACCURATELY THEIR INCIDENCE OR OUTCOME. HOWEVER, THE VAST MAJORITY OF THE CASES OF LEUKOPENIA HAVE NOT PROGRESSED TO THE MORE SERIOUS CONDITIONS OF APLASTIC ANEMIA OR AGRANULOCYTOSIS.
BECAUSE OF THE VERY LOW INCIDENCE OF AGRANULOCYTOSIS AND APLASTIC ANEMIA, THE VAST MAJORITY OF MINOR HEMATOLOGIC CHANGES OBSERVED IN MONITORING OF PATIENTS ON CARBAMAZEPINE ARE UNLIKELY TO SIGNAL THE OCCURRENCE OF EITHER ABNORMALITY. NONETHELESS, COMPLETE PRETREATMENT HEMATOLOGICAL TESTING SHOULD BE OBTAINED AS A BASELINE. IF A PATIENT IN THE COURSE OF TREATMENT EXHIBITS LOW OR DECREASED WHITE BLOOD CELL OR PLATELET COUNTS, THE PATIENT SHOULD BE MONITORED CLOSELY. DISCONTINUATION OF THE DRUG SHOULD BE CONSIDERED IF ANY EVIDENCE OF SIGNIFICANT BONE MARROW DEPRESSION DEVELOPS.
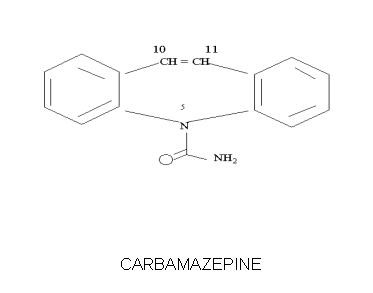
1DESCRIPTION
CARBATROL is an anticonvulsant and specific analgesic for trigeminal neuralgia, available for oral administration as 100 mg, 200 mg and 300 mg extended-release capsules of Carbamazepine, USP. Carbamazepine is a white to off-white powder, practically insoluble in water and soluble in alcohol and in acetone. Its molecular weight is 236.27. Its chemical name is 5H-dibenz[b,f]azepine-5-carboxamide, and its structural formula is:
Carbatrol is a multi-component capsule formulation consisting of three different types of beads: immediate-release beads, extended-release beads, and enteric-release beads. The three bead types are combined in a specific ratio to provide twice daily dosing of Carbatrol.
Inactive ingredients: citric acid, colloidal silicon dioxide, lactose monohydrate, microcrystalline cellulose, polyethylene glycol, povidone, sodium lauryl sulfate, talc, triethyl citrate and other ingredients.
The 100 mg capsule shells contain gelatin-NF, FD&C Blue #2, Yellow Iron Oxide, and titanium dioxide and are imprinted with white ink; the 200 mg capsule shells contain gelatin-NF, FD&C Red #3, FD&C Yellow #6, Yellow Iron Oxide, FD&C Blue #2, and titanium dioxide, and are imprinted with white ink; and the 300 mg capsule shells contain gelatin-NF, FD&C Blue #2, FD&C Yellow #6, Red Iron Oxide, Yellow Iron Oxide, and titanium dioxide, and are imprinted with white ink.
2CLINICAL PHARMACOLOGY
In controlled clinical trials, carbamazepine has been shown to be effective in the treatment of psychomotor and grand mal seizures, as well as trigeminal neuralgia.
2.1Mechanism of Action
Carbamazepine has demonstrated anticonvulsant properties in rats and mice with electrically and chemically induced seizures. It appears to act by reducing polysynaptic responses and blocking the post-tetanic potentiation. Carbamazepine greatly reduces or abolishes pain induced by stimulation of the infraorbital nerve in cats and rats. It depresses thalamic potential and bulbar and polysynaptic reflexes, including the linguomandibular reflex in cats. Carbamazepine is chemically unrelated to other anticonvulsants or other drugs used to control the pain of trigeminal neuralgia. The mechanism of action remains unknown.
The principal metabolite of carbamazepine, carbamazepine-10,11-epoxide, has anticonvulsant activity as demonstrated in several
2.2Pharmacokinetics
Carbamazepine (CBZ): Taken every 12 hours, carbamazepine extended-release capsules provide steady state plasma levels comparable to immediate-release carbamazepine tablets given every 6 hours, when administered at the same total mg daily dose.
Following a single 200 mg oral extended-release dose of carbamazepine, peak plasma concentration was 1.9 ± 0.3 μg/mL and the time to reach the peak was 19 ± 7 hours. Following chronic administration (800 mg every 12 hours), the peak levels were 11.0 ± 2.5 μg/mL and the time to reach the peak was 5.9 ± 1.8 hours. The pharmacokinetics of extended-release carbamazepine is linear over the single dose range of 200-800 mg.
Carbamazepine is 76% bound to plasma proteins. Carbamazepine is primarily metabolized in the liver. Cytochrome P450 3A4 was identified as the major isoform responsible for the formation of carbamazepine-10,11-epoxide. Since carbamazepine induces its own metabolism, the half-life is also variable. Following a single extended-release dose of carbamazepine, the average half-life range from 35-40 hours and 12-17 hours on repeated dosing. The apparent oral clearance following a single dose was 25 ± 5 mL/min and following multiple dosing was 80 ± 30 mL/min.
After oral administration of 14C-carbamazepine, 72% of the administered radioactivity was found in the urine and 28% in the feces. This urinary radioactivity was composed largely of hydroxylated and conjugated metabolites, with only 3% of unchanged carbamazepine.
Carbamazepine-10,11-epoxide (CBZ-E): Carbamazepine-10,11-epoxide is considered to be an active metabolite of carbamazepine. Following a single 200 mg oral extended-release dose of carbamazepine, the peak plasma concentration of carbamazepine-10,11-epoxide was 0.11 ± 0.012 μg/mL and the time to reach the peak was 36 ± 6 hours. Following chronic administration of an extended-release dose of carbamazepine (800 mg every 12 hours), the peak levels of carbamazepine-10,11-epoxide were 2.2 ± 0.9 μg/mL and the time to reach the peak was 14 ± 8 hours. The plasma half-life of carbamazepine-10,11-epoxide following administration of carbamazepine is 34 ± 9 hours. Following a single oral dose of extended-release carbamazepine (200-800 mg) the AUC and Cmax of carbamazepine-10,11-epoxide were less than 10% of carbamazepine. Following multiple dosing of extended-release carbamazepine (800-1600 mg daily for 14 days), the AUC and Cmax of carbamazepine-10,11-epoxide were dose related, ranging from 15.7 μg.hr/mL and 1.5 μg/mL at 800 mg/day to 32.6 μg.hr/mL and 3.2 μg/mL at 1600 mg/day, respectively, and were less than 30% of carbamazepine. Carbamazepine-10,11-epoxide is 50% bound to plasma proteins.
Food Effect: A high fat meal diet increased the rate of absorption of a single 400 mg dose (mean Tmax was reduced from 24 hours, in the fasting state, to 14 hours and Cmax increased from 3.2 to 4.3 μg/mL) but not the extent (AUC) of absorption. The elimination half-life remains unchanged between fed and fasting state. The multiple dose study conducted in the fed state showed that the steady-state Cmax values were within the therapeutic concentration range. The pharmacokinetic profile of extended-release carbamazepine was similar when given by sprinkling the beads over applesauce compared to the intact capsule administered in the fasted state.
2.3Special Populations
Hepatic Dysfunction: The effect of hepatic impairment on the pharmacokinetics of carbamazepine is not known. However, given that carbamazepine is primarily metabolized in the liver, it is prudent to proceed with caution in patients with hepatic dysfunction.
Renal Dysfunction: The effect of renal impairment on the pharmacokinetics of carbamazepine is not known.
Gender: No difference in the mean AUC and Cmax of carbamazepine and carbamazepine-10,11-epoxide was found between males and females.
Age: Carbamazepine is more rapidly metabolized to carbamazepine-10,11-epoxide in young children than adults. In children below the age of 15, there is an inverse relationship between CBZ-E/CBZ ratio and increasing age.
Race: No information is available on the effect of race on the pharmacokinetics of carbamazepine.
3CONTRAINDICATIONS
Carbamazepine should not be used in patients with a history of previous bone marrow depression, hypersensitivity to the drug, or known sensitivity to any of the tricyclic compounds, such as amitriptyline, desipramine, imipramine, protriptyline and nortriptyline. Likewise, on theoretical grounds its use with monoamine oxidase inhibitors is not recommended. Before administration of carbamazepine, MAO inhibitors should be discontinued for a minimum of 14 days, or longer if the clinical situation permits.
Coadministration of carbamazepine and nefazodone may result in insufficient plasma concentrations of nefazodone and its active metabolite to achieve a therapeutic effect. Coadministration of carbamazepine with nefazodone is contraindicated.
Coadministration of Carbatrol is contraindicated with delavirdine due to the potential for loss of virologic response and possible resistance to delavirdine or to the class of non-nucleoside reverse transcriptase inhibitors.
4ADVERSE REACTIONS
General: If adverse reactions are of such severity that the drug must be discontinued, the physician must be aware that abrupt discontinuation of any anticonvulsant drug in a responsive patient with epilepsy may lead to seizures or even status epilepticus with its life-threatening hazards.
The most severe adverse reactions previously observed with carbamazepine were reported in the hemopoietic system and skin (see
The most frequently observed adverse reactions, particularly during the initial phases of therapy, are dizziness, drowsiness, unsteadiness, nausea, and vomiting. To minimize the possibility of such reactions, therapy should be initiated at the lowest dosage recommended.
The following additional adverse reactions were previously reported with carbamazepine:
Hemopoietic System: Aplastic anemia, agranulocytosis, pancytopenia, bone marrow depression, thrombocytopenia, leukopenia, leukocytosis, eosinophilia, acute intermittent porphyria.
Skin: Toxic epidermal necrolysis (TEN) and Stevens-Johnson syndrome (SJS) (see BOXED WARNING), Acute Generalized Exanthematous Pustulosis (AGEP), pruritic and erythematous rashes, urticaria, photosensitivity reactions, alterations in skin pigmentation, exfoliative dermatitis, erythema multiforme and nodosum, purpura, aggravation of disseminated lupus erythematosus, alopecia, diaphoresis, onychomadesis and hirsutism. In certain cases, discontinuation of therapy may be necessary.
Cardiovascular System: Congestive heart failure, edema, aggravation of hypertension, hypotension, syncope and collapse, aggravation of coronary artery disease, arrhythmias and AV block, thrombophlebitis, thromboembolism, and adenopathy or lymphadenopathy. Some of these cardiovascular complications have resulted in fatalities. Myocardial infarction has been associated with other tricyclic compounds.
Immune system disorders: Hypogammaglobulinemia.
Liver: Abnormalities in liver function tests, cholestatic and hepatocellular jaundice, hepatitis, and hepatic failure.
Pancreatic: Pancreatitis.
Respiratory System: Pulmonary hypersensitivity characterized by fever, dyspnea, pneumonitis, or pneumonia.
Genitourinary System: Urinary frequency, acute urinary retention, oliguria with elevated blood pressure, azotemia, renal failure, and impotence. Albuminuria, glycosuria, elevated BUN, and microscopic deposits in the urine have also been reported. There have been rare reports of impaired male fertility and/or abnormal spermatogenesis.
Testicular atrophy occurred in rats receiving carbamazepine orally from 4-52 weeks at dosage levels of 50-400 mg/kg/day. Additionally, rats receiving carbamazepine in the diet for 2 years at dosage levels of 25, 75, and 250 mg/kg/day had a dose-related incidence of testicular atrophy and aspermatogenesis. In dogs, it produced a brownish discoloration, presumably a metabolite, in the urinary bladder at dosage levels of 50 mg/kg/day and higher. Relevance of these findings to humans is unknown.
Nervous System: Dizziness, drowsiness, disturbances of coordination, confusion, headache, fatigue, blurred vision, visual hallucinations, transient diplopia, oculomotor disturbances, nystagmus, speech disturbances, abnormal involuntary movements, peripheral neuritis and paresthesias, depression with agitation, talkativeness, tinnitus, and hyperacusis.
There have been reports of associated paralysis and other symptoms of cerebral arterial insufficiency, but the exact relationship of these reactions to the drug has not been established.
Isolated cases of neuroleptic malignant syndrome have been reported with concomitant use of psychotropic drugs.
Digestive System: Nausea, vomiting, gastric distress and abdominal pain, diarrhea, constipation, anorexia, and dryness of the mouth and pharynx, including glossitis and stomatitis.
Eyes: Scattered punctate cortical lens opacities, as well as conjunctivitis, have been reported. Although a direct causal relationship has not been established, many phenothiazines and related drugs have been shown to cause eye changes.
Musculoskeletal System: Bone loss, aching joints and muscles, and leg cramps.
Metabolism: Fever and chills, decreased levels of plasma calcium leading to osteoporosis, and hyperammonemia have been reported.
Other: Isolated cases of a lupus erythematosus-like syndrome have been reported. There have been occasional reports of elevated levels of cholesterol, HDL cholesterol, and triglycerides in patients taking anticonvulsants.
A case of aseptic meningitis, accompanied by myoclonus and peripheral eosinophilia, has been reported in a patient taking carbamazepine in combination with other medications. The patient was successfully dechallenged, and the meningitis reappeared upon rechallenge with carbamazepine.
5DRUG ABUSE AND DEPENDENCE
No evidence of abuse potential has been associated with carbamazepine, nor is there evidence of psychological or physical dependence in humans.
6DOSAGE AND ADMINISTRATION
Monitoring of blood levels has increased the efficacy and safety of anticonvulsants (see
Carbatrol is an extended-release formulation for twice a day administration. When converting patients from immediate release carbamazepine to Carbatrol extended-release capsules, the same total daily mg dose of carbamazepine should be administered. Following conversion to Carbatrol, patients should be closely monitored for seizure control. Depending on the therapeutic response after conversion, the total daily dose may need to be adjusted within the recommended dosing instructions.
Epilepsy (see
Adults and children over 12 years of age. Initial: 200 mg twice daily. Increase at weekly intervals by adding up to 200 mg/day until the optimal response is obtained. Dosage generally should not exceed 1000 mg per day in children 12-15 years of age, and 1200 mg daily in patients above 15 years of age. Doses up to 1600 mg daily have been used in adults. Maintenance: Adjust dosage to the minimum effective level, usually 800-1200 mg daily.
Children under 12 years of age: Children taking total daily dosages of immediate-release carbamazepine of 400 mg or greater may be converted to the same total daily dosage of Carbatrol extended-release capsules, using a twice daily regimen. Ordinarily, optimal clinical response is achieved at daily doses below 35 mg/kg. If satisfactory clinical response has not been achieved, plasma levels should be measured to determine whether or not they are in the therapeutic range. No recommendation regarding the safety of Carbatrol for use at doses above 35 mg/kg/24 hours can be made.
Combination Therapy: Carbatrol may be used alone or with other anticonvulsants. When added to existing anticonvulsant therapy, the drug should be added gradually while the other anticonvulsants are maintained or gradually decreased, except phenytoin, which may have to be increased (see PRECAUTIONS, Drug Interactions).
Trigeminal Neuralgia (see
Initial: On the first day, start with one 200 mg capsule. This daily dose may be increased by up to 200 mg/day every 12 hours only as needed to achieve freedom from pain. Do not exceed 1200 mg daily.
Maintenance: Control of pain can be maintained in most patients with 400-800 mg daily. However, some patients may be maintained on as little as 200 mg daily, while others may require as much as 1200 mg daily. At least once every 3 months throughout the treatment period, attempts should be made to reduce the dose to the minimum effective level or even to discontinue the drug.
7HOW SUPPLIED
Carbatrol (carbamazepine) extended-release capsules is supplied in three dosage strengths.
100 mg-Two-piece hard gelatin capsule (bluish green opaque body and cap) printed with the Shire logo in white ink.
Supplied in bottles of 120........................... NDC 54092-171-12
200 mg-Two-piece hard gelatin capsule (light gray opaque body with bluish green opaque cap) printed with the Shire logo in white ink.
Supplied in bottles of 120 ............................NDC 54092-172-12
300 mg-Two-piece hard gelatin capsule (black opaque body with bluish green opaque cap) printed with the Shire logo in white ink.
Supplied in bottles of 120 ............................NDC 54092-173-12
Store at 25°C (77°F); excursions permitted to 15-30°C (59-86°F) [see USP controlled room temperature]. PROTECT FROM LIGHT AND MOISTURE.
To report SUSPECTED ADVERSE REACTIONS, contact Takeda Pharmaceuticals at 1-800-828-2088 or FDA at 1-800-FDA-1088 or
Distributed by:
CARBATROL is a registered trademark of Takeda Pharmaceuticals U.S.A., Inc.
© 2025 Takeda Pharmaceuticals U.S.A., Inc. All rights reserved.
Rev 6/2025
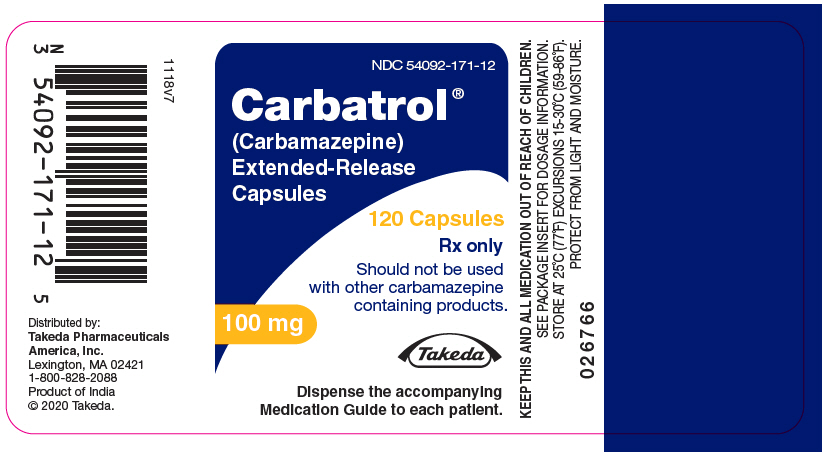
8PRINCIPAL DISPLAY PANEL - 100 mg Capsule Bottle Label
NDC 54092-171-12
Carbatrol ®
120 Capsules
Rx only
Should not be used
with other carbamazepine
containing products.
Should not be used
with other carbamazepine
containing products.
100 mg
Takeda
Dispense the accompanying
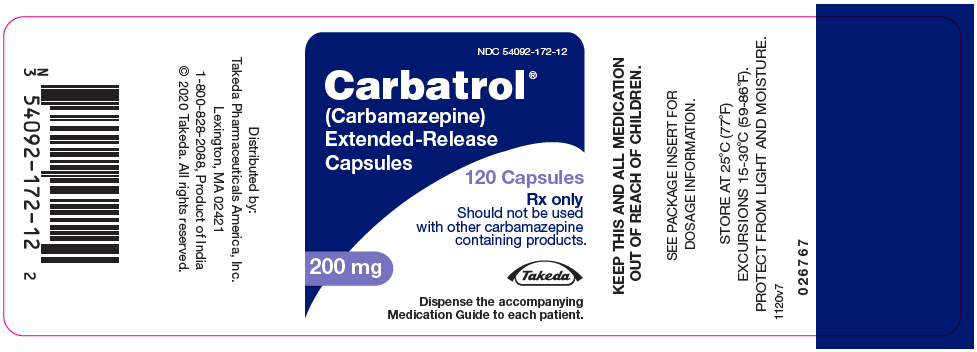
9PRINCIPAL DISPLAY PANEL - 200 mg Capsule Bottle Label
NDC 54092-172-12
Carbatrol
120 Capsules
Rx only
Should not be used
with other carbamazepine
containing products.
Should not be used
with other carbamazepine
containing products.
200 mg
Takeda
Dispense the accompanying
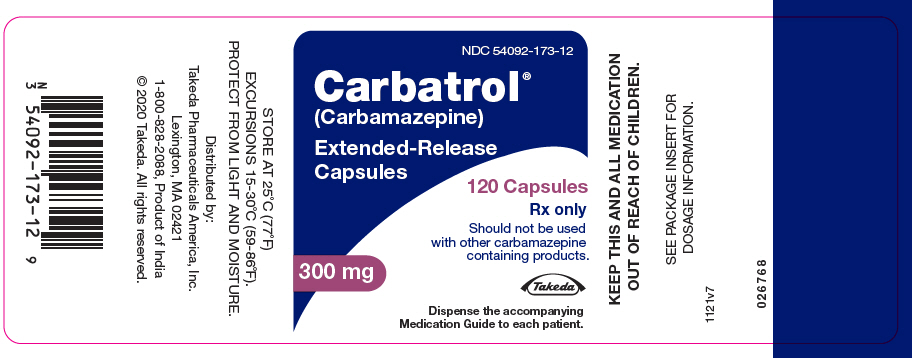
10PRINCIPAL DISPLAY PANEL - 300 mg Capsule Bottle Label
NDC 54092-173-12
Carbatrol
120 Capsules
Rx only
Should not be used
with other carbamazepine
containing products.
Should not be used
with other carbamazepine
containing products.
300 mg
Takeda
Dispense the accompanying