Generic Name
Lorazepam
Brand Names
Ativan, Loreev
FDA approval date: July 25, 1980
Classification: Benzodiazepine
Form: Liquid, Injection, Concentrate, Tablet, Capsule, Solution
What is Ativan (Lorazepam)?
Lorazepam is indicated for the management of anxiety disorders or for the short-term relief of the symptoms of anxiety or anxiety associated with depressive symptoms. Anxiety or tension associated with the stress of everyday life usually does not require treatment with an anxiolytic. The effectiveness of lorazepam in long-term use, that is, more than 4 months, has not been assessed by systematic clinical studies. The physician should periodically reassess the usefulness of the drug for the individual patient.
Approved To Treat
Top Global Experts
There are no experts for this drug
Save this treatment for later
Not sure about your diagnosis?
Related Clinical Trials
There is no clinical trials being done for this treatment
Related Latest Advances
There is no latest advances for this treatment
Brand Information
Ativan (Lorazepam)
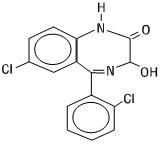
1DESCRIPTION
Lorazepam, a benzodiazepine with antianxiety, sedative, and anticonvulsant effects, is intended for the intramuscular or intravenous routes of administration. It has the chemical formula: 7-chloro-5(2-chlorophenyl)-1,3-dihydro-3-hydroxy-2
Lorazepam is a nearly white powder almost insoluble in water. Each mL of sterile injection contains either 2.0 or 4.0 mg of lorazepam, 0.18 mL polyethylene glycol 400 in propylene glycol with 2.0% benzyl alcohol as preservative.
2CLINICAL PHARMACOLOGY
Lorazepam interacts with the γ-aminobutyric acid (GABA)-benzodiazepine receptor complex, which is widespread in the brain of humans as well as other species. This interaction is presumed to be responsible for lorazepam’s mechanism of action. Lorazepam exhibits relatively high and specific affinity for its recognition site but does not displace GABA. Attachment to the specific binding site enhances the affinity of GABA for its receptor site on the same receptor complex. The pharmacodynamic consequences of benzodiazepine agonist actions include antianxiety effects, sedation, and reduction of seizure activity. The intensity of action is directly related to the degree of benzodiazepine receptor occupancy.
2.1Effects in Pre-Operative Patients
Intravenous or intramuscular administration of the recommended dose of 2 mg to 4 mg of ATIVAN Injection to adult patients is followed by dose-related effects of sedation (sleepiness or drowsiness), relief of preoperative anxiety, and lack of recall of events related to the day of surgery in the majority of patients. The clinical sedation (sleepiness or drowsiness) thus noted is such that the majority of patients are able to respond to simple instructions whether they give the appearance of being awake or asleep. The lack of recall is relative rather than absolute, as determined under conditions of careful patient questioning and testing, using props designed to enhance recall. The majority of patients under these reinforced conditions had difficulty recalling perioperative events or recognizing props from before surgery. The lack of recall and recognition was optimum within 2 hours following intramuscular administration and 15 to 20 minutes after intravenous injection.
The intended effects of the recommended adult dose of ATIVAN Injection usually last 6 to 8 hours. In rare instances, and where patients received greater than the recommended dose, excessive sleepiness and prolonged lack of recall were noted. As with other benzodiazepines, unsteadiness, enhanced sensitivity to CNS-depressant effects of ethyl alcohol and other drugs were noted in isolated and rare cases for greater than 24 hours.
2.2Physiologic Effects in Healthy Adults
Studies in healthy adult volunteers reveal that intravenous lorazepam in doses up to 3.5 mg/70 kg does not alter sensitivity to the respiratory stimulating effect of carbon dioxide and does not enhance the respiratory-depressant effects of doses of meperidine up to 100 mg/70 kg (also determined by carbon dioxide challenge) as long as patients remain sufficiently awake to undergo testing. Upper airway obstruction has been observed in rare instances where the patient received greater than the recommended dose and was excessively sleepy and difficult to arouse (see
Clinically employed doses of ATIVAN Injection do not greatly affect the circulatory system in the supine position or employing a 70-degree tilt test. Doses of 8 mg to 10 mg of intravenous lorazepam (2 to 2-1/2 times the maximum recommended dosage) will produce loss of lid reflexes within 15 minutes.
Studies in 6 healthy young adults who received lorazepam injection and no other drugs revealed that visual tracking (the ability to keep a moving line centered) was impaired for a mean of 8 hours following administration of 4 mg of intramuscular lorazepam and 4 hours following administration of 2 mg intramuscularly with considerable subject variation. Similar findings were noted with pentobarbital, 150 and 75 mg. Although this study showed that both lorazepam and pentobarbital interfered with eye-hand coordination, the data are insufficient to predict when it would be safe to operate a motor vehicle or engage in a hazardous occupation or sport.
2.3Clinical Studies
The effectiveness of ATIVAN Injection in status epilepticus was established in two multi-center controlled trials in 177 patients. With rare exceptions, patients were between 18 and 65 years of age. More than half the patients in each study had tonic-clonic status epilepticus; patients with simple partial and complex partial status epilepticus comprised the rest of the population studied, along with a smaller number of patients who had absence status.
One study (n=58) was a double-blind active-control trial comparing ATIVAN Injection and diazepam. Patients were randomized to receive ATIVAN 2 mg IV (with an additional 2 mg IV if needed) or diazepam 5 mg IV (with an additional 5 mg IV if needed). The primary outcome measure was a comparison of the proportion of responders in each treatment group, where a responder was defined as a patient whose seizures stopped within 10 minutes after treatment and who continued seizure-free for at least an additional 30 minutes. Twenty-four of the 30 (80%) patients were deemed responders to ATIVAN and 16/28 (57%) patients were deemed responders to diazepam (p=0.04). Of the 24 ATIVAN responders, 23 received both 2 mg infusions.
Non-responders to ATIVAN 4 mg were given an additional 2 to 4 mg ATIVAN; non-responders to diazepam 10 mg were given an additional 5 to 10 mg diazepam. After this additional dose administration, 28/30 (93%) of patients randomized to ATIVAN and 24/28 (86%) of patients randomized to diazepam were deemed responders, a difference that was not statistically significant.
Although this study provides support for the efficacy of ATIVAN as the treatment for status epilepticus, it cannot speak reliably or meaningfully to the comparative performance of either diazepam (Valium) or lorazepam (ATIVAN Injection) under the conditions of actual use.
A second study (n=119) was a double-blind dose-comparison trial with 3 doses of ATIVAN Injection: 1 mg, 2 mg, and 4 mg. Patients were randomized to receive one of the three doses of ATIVAN. The primary outcome and definition of responder were as in the first study. Twenty-five of 41 patients (61%) responded to 1 mg ATIVAN; 21/37 patients (57%) responded to 2 mg ATIVAN; and 31/41 (76%) responded to 4 mg ATIVAN. The p-value for a statistical test of the difference between the ATIVAN 4 mg dose group and the ATIVAN 1-mg dose group was 0.08 (two-sided). Data from all randomized patients were used in this test.
Although analyses failed to detect an effect of age, sex, or race on the effectiveness of ATIVAN in status epilepticus, the numbers of patients evaluated were too few to allow a definitive conclusion about the role these factors may play.
3CONTRAINDICATIONS
ATIVAN Injection is contraindicated in patients with a known sensitivity to benzodiazepines or its vehicle (polyethylene glycol, propylene glycol, and benzyl alcohol), in patients with acute narrow-angle glaucoma, or in patients with sleep apnea syndrome. It is also contraindicated in patients with severe respiratory insufficiency, except in those patients requiring relief of anxiety and/or diminished recall of events while being mechanically ventilated. The use of ATIVAN Injection intra-arterially is contraindicated because, as with other injectable benzodiazepines, inadvertent intra-arterial injection may produce arteriospasm resulting in gangrene which may require amputation (see
ATIVAN Injection is contraindicated for use in premature infants because the formulation contains benzyl alcohol (see
4OVERDOSAGE
Overdosage of benzodiazepines is characterized by central nervous system depression ranging from drowsiness to coma. In mild to moderate cases, symptoms can include drowsiness, confusion, dysarthria, lethargy, hypnotic state, diminished reflexes, ataxia, and hypotonia.. Rarely, paradoxical or disinhibitory reactions (including agitation, irritability, impulsivity, violent behavior, confusion, restlessness, excitement, and talkativeness) may occur. In severe overdosage cases, patients may develop respiratory depression and coma. Overdosage of benzodiazepines in combination with other CNS depressants (including alcohol and opioids) may be fatal (see
In managing benzodiazepine overdosage, employ general supportive measures, including intravenous fluids and airway management. Flumazenil, a specific benzodiazepine receptor antagonist indicated for the complete or partial reversal of the sedative effects of benzodiazepines in the management of benzodiazepine overdosage, can lead to withdrawal and adverse reactions, including seizures, particularly in the context of mixed overdosage with drugs that increase seizure risk (e.g., tricyclic and tetracyclic antidepressants) and in patients with long-term benzodiazepine use and physical dependency. The risk of withdrawal seizures with flumazenil use may be increased in patients with epilepsy. Flumazenil is contraindicated in patients who have received a benzodiazepine for control of a potentially life-threatening condition (e.g., status epilepticus). If the decision is made to use flumazenil, it should be used as an adjunct to, not as a substitute for, supportive management of benzodiazepine overdosage. See the flumazenil Injection Prescribing Information.
Consider contacting
5DOSAGE AND ADMINISTRATION
NOTE: CONTAINS BENZYL ALCOHOL (see
ATIVAN must never be used without individualization of dosage particularly when used with other medications capable of producing central-nervous-system depression.
EQUIPMENT NECESSARY TO MAINTAIN A PATENT AIRWAY SHOULD BE IMMEDIATELY AVAILABLE PRIOR TO INTRAVENOUS ADMINISTRATION OF LORAZEPAM (see
5.1Administration
When given intramuscularly, ATIVAN Injection, undiluted, should be injected deep in the muscle mass.
Injectable ATIVAN can be used with atropine sulfate, narcotic analgesics, other parenterally used analgesics, commonly used anesthetics, and muscle relaxants.
Immediately prior to intravenous use, ATIVAN Injection must be diluted with an equal volume of compatible solution. Contents should be mixed thoroughly by gently inverting the container repeatedly until a homogenous solution results. Do not shake vigorously, as this will result in air entrapment. When properly diluted, the drug may be injected directly into a vein or into the tubing of an existing intravenous infusion. The rate of injection should not exceed 2.0 mg per minute.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. Do not use if solution is discolored or contains a precipitate.
ATIVAN Injection is compatible for dilution purposes with the following solutions: Sterile Water for Injection, USP; Sodium Chloride Injection, USP; 5% Dextrose Injection, USP.
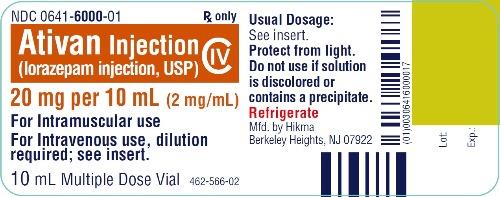
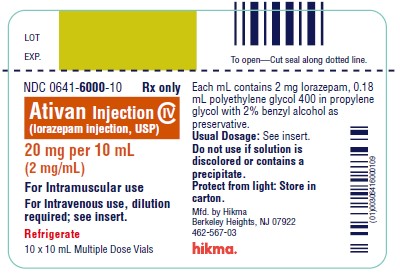
6HOW SUPPLIED
ATIVAN Injection (lorazepam injection, USP) is available in the following dosage strengths in single-dose and multiple-dose vials:
2 mg per mL, NDC 0641-6001-25, 25 x 1 mL vial
For IM or IV injection.Store in a refrigerator.PROTECT FROM LIGHT.Use carton to protect contents from light.
7ANIMAL TOXICOLOGY AND/OR PHARMACOLOGY
Published studies in animals demonstrate that the use of anesthetic agents during the period of rapid brain growth or synaptogenesis results in widespread neuronal and oligodendrocyte cell loss in the developing brain and alterations in synaptic morphology and neurogenesis. Based on comparisons across species, the window of vulnerability to these changes is believed to correlate with exposures in the third trimester through the first several months of life, but may extend out to approximately 3 years of age in humans.
In primates, exposure to 3 hours of an anesthetic regimen that produced a light surgical plane of anesthesia did not increase neuronal cell loss, however, treatment regimens of 5 hours or longer increased neuronal cell loss. Data in rodents and in primates suggest that the neuronal and oligodendrocyte cell losses are associated with subtle but prolonged cognitive deficits in learning and memory. The clinical significance of these nonclinical findings is not known, and healthcare providers should balance the benefits of appropriate anesthesia in neonates and young children who require procedures against the potential risks suggested by the nonclinical data (see
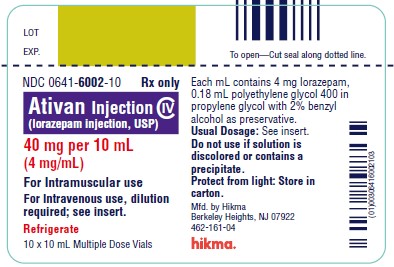
8PRINCIPAL DISPLAY PANEL
NDC 0641-

NDC 0641-

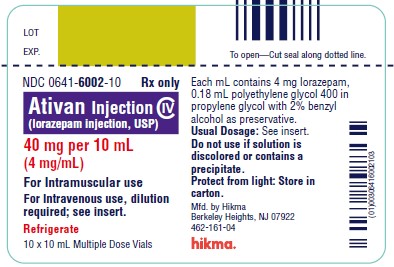
9PRINCIPAL DISPLAY PANEL
NDC 0641-
NDC 0641-
10PRINCIPAL DISPLAY PANEL
NDC 0641-

NDC 0641-
11PRINCIPAL DISPLAY PANEL
NDC 0641-

NDC 0641-
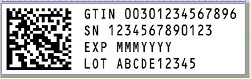
12SERIALIZATION IMAGE