Generic Name
Clobazam
Brand Names
Onfi, Sympazan
FDA approval date: December 14, 2012
Classification: Benzodiazepine
Form: Tablet, Film, Suspension
What is Onfi (Clobazam)?
Clobazam tablets are indicated for the adjunctive treatment of seizures associated with Lennox-Gastaut syndrome in patients 2 years of age or older. Clobazam is a benzodiazepine indicated for adjunctive treatment of seizures associated with Lennox-Gastaut syndrome in patients 2 years of age or older
Approved To Treat
Top Global Experts
There are no experts for this drug
Save this treatment for later
Not sure about your diagnosis?
Related Clinical Trials
There is no clinical trials being done for this treatment
Related Latest Advances
There is no latest advances for this treatment
Brand Information
Onfi (clobazam)
WARNING: RISKS FROM CONCOMITANT USE WITH OPIOIDS; ABUSE,MISUSE, AND ADDICTION; and DEPENDENCE AND WITHDRAWAL REACTIONS
- Concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing of these drugs for patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Follow patients for signs and symptoms of respiratory depression and sedation [see Warnings and Precautions (.
- The use of benzodiazepines, including ONFI, exposes users to risks of abuse, misuse, and addiction, which can lead to overdose or death. Abuse and misuse of benzodiazepines commonly involve concomitant use of other medications, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse outcomes. Before prescribing ONFI and throughout treatment, assess each patient’s risk for abuse, misuse, and addiction .
- The continued use of benzodiazepines, including ONFI, may lead to clinically significant physical dependence. .
1INDICATIONS AND USAGE
ONFI
2DOSAGE FORMS AND STRENGTHS
Tablets: 10 mg and 20 mg with a functional score for oral administration.
Oral Suspension: 2.5 mg/mL for oral administration. Each bottle contains 120 mL of an off-white suspension.
3CONTRAINDICATIONS
ONFI iscontraindicated in patients with a history of hypersensitivity to the drug orits ingredients. Hypersensitivity reactions have included seriousdermatological reactions
4ADVERSE REACTIONS
Clinically significant adverse reactions that appear in other sections of the labeling include the following:
- Risks from Concomitant Use with Opioids
- Abuse, Misuse, and Addiction
- Dependence and Withdrawal Reactions
- Potentiation of Sedation from Concomitant Use with Central Nervous System Depressants
- Somnolence or Sedation
- Serious Dermatological Reactions
- Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS)/Multiorgan Hypersensitivity
- Suicidal Behavior and Ideation
- Neonatal Sedation and Withdrawal Syndrome
4.1Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
During its development for the adjunctive treatment of seizures associated with LGS, ONFI was administered to 333 healthy volunteers and 300 patients with a current or prior diagnosis of LGS, including 197 patients treated for 12 months or more. The conditions and duration of exposure varied greatly and included single- and multiple-dose clinical pharmacology studies in healthy volunteers and two double-blind studies in patients with LGS (Study 1 and 2)
Adverse Reactions Leading to Discontinuation in an LGS Placebo Controlled Clinical Trial (Study 1)The adverse reactions associated with ONFI treatment discontinuation in ≥1% of patients in decreasing order of frequency included lethargy, somnolence, ataxia, aggression, fatigue, and insomnia.
Most Common Adverse Reactions in an LGS Placebo Controlled Clinical Trial (Study 1)Table 3 lists the adverse reactions that occurred in ≥5% of ONFI-treated patients (at any dose), and at a rate greater than placebo-treated patients, in the randomized, double-blind, placebo-controlled, parallel group clinical study of adjunctive AED therapy for 15 weeks (Study 1).
4.2Postmarketing Experience
These reactions are reported voluntarily from a population of uncertain size; therefore, it is not possible to estimate their frequency or establish a causal relationship to drug exposure. Adverse reactions are categorized by system organ class.
Blood Disorders: Anemia, eosinophilia, leukopenia, thrombocytopenia
Eye Disorders: Diplopia, vision blurred
Gastrointestinal Disorders: Abdominal distention
General Disorders and Administration Site Conditions: Hypothermia
Investigations: Hepatic enzyme increased
Musculoskeletal: Muscle spasms
Psychiatric Disorders: Agitation, anxiety, apathy, confusional state, depression, delirium, delusion, hallucination
Renal and Urinary Disorders: Urinary retention
Respiratory Disorders: Aspiration, respiratory depression
Skin and Subcutaneous Tissue Disorders: Rash, urticaria, angioedema, and facial and lip edema
Eye Disorders: Diplopia, vision blurred
Gastrointestinal Disorders: Abdominal distention
General Disorders and Administration Site Conditions: Hypothermia
Investigations: Hepatic enzyme increased
Musculoskeletal: Muscle spasms
Psychiatric Disorders: Agitation, anxiety, apathy, confusional state, depression, delirium, delusion, hallucination
Renal and Urinary Disorders: Urinary retention
Respiratory Disorders: Aspiration, respiratory depression
Skin and Subcutaneous Tissue Disorders: Rash, urticaria, angioedema, and facial and lip edema
5OVERDOSAGE
Overdosage of benzodiazepines is characterized by central nervous system depression ranging from drowsiness to coma. In mild to moderate cases, symptoms can include drowsiness, confusion, dysarthria, lethargy, hypnotic state, diminished reflexes, ataxia, and hypotonia. Rarely, paradoxical or disinhibitory reactions (including agitation, irritability, impulsivity, violent behavior, confusion, restlessness, excitement, and talkativeness) may occur. In severe overdosage cases, patients may develop respiratory depression and coma. Overdosage of benzodiazepines in combination with other CNS depressants (including alcohol and opioids) may be fatal
In managing benzodiazepine overdosage, employ general supportive measures, including intravenous fluids and airway maintenance. Flumazenil, a specific benzodiazepine receptor antagonist indicated for the complete or partial reversal of the sedative effects of benzodiazepines in the management of benzodiazepine overdosage, can lead to withdrawal and adverse reactions, including seizures, particularly in the context of mixed overdosage with drugs that increase seizure risk (e.g., tricyclic and tetracyclic antidepressants) and in patients with long-term benzodiazepine use and physical dependency. The risk of withdrawal seizures with flumazenil may be increased in patients with epilepsy. Flumazenil is contraindicated in patients who have received a benzodiazepine for control of a potentially life-threatening condition (e.g., status epilepticus). If the decision is made to use flumazenil, it should be used as an adjunct to, not as a substitute for, supportive management of benzodiazepine overdosage. See the flumazenil injection Prescribing Information.
Consider contacting the Poison Help line (1-800-222-1222) or a medical toxicologist for additional overdosage management recommendations.
6DESCRIPTION
Clobazam is a white or almost white, crystalline powder with a slightly bitter taste; is slightly soluble in water, sparingly soluble in ethanol, and freely soluble in methylene chloride. The melting range of clobazam is from 182ºC to 185ºC. The molecular formula is C
Each ONFI tablet contains 10 mg or 20 mg of clobazam. Tablets also contain as inactive ingredients: modified corn starch, lactose monohydrate, magnesium stearate, silicon dioxide, and talc.
ONFI is also available for oral administration as an off-white suspension containing clobazam at a concentration of 2.5 mg/mL. Inactive ingredients include magnesium aluminum silicate, xanthan gum, citric acid monohydrate, disodium hydrogen phosphate dihydrate, simethicone emulsion, polysorbate 80, methylparaben, propylparaben, propylene glycol, sucralose, maltitol solution, berry flavor, purified water.
7CLINICAL STUDIES
The effectiveness of ONFI for the adjunctive treatment of seizures associated with Lennox-Gastaut syndrome was established in two multicenter controlled studies (Study 1 and Study 2). Both studies were similar in terms of disease characteristics and concomitant AED treatments. The most common concomitant AED treatments at baseline included: valproate, lamotrigine, levetiracetam, and topiramate.
Study 1
Study 1 (N=238) was a randomized, double-blind, placebo-controlled study consisting of a 4-week baseline period followed by a 3-week titration period and 12-week maintenance period. Patients age 2-54 years with a current or prior diagnosis of LGS were stratified into 2 weight groups (12.5 kg to ≤30 kg or >30 kg) and then randomized to placebo or one of three target maintenance doses of ONFI according to Table 5.
Study 1 (N=238) was a randomized, double-blind, placebo-controlled study consisting of a 4-week baseline period followed by a 3-week titration period and 12-week maintenance period. Patients age 2-54 years with a current or prior diagnosis of LGS were stratified into 2 weight groups (12.5 kg to ≤30 kg or >30 kg) and then randomized to placebo or one of three target maintenance doses of ONFI according to Table 5.
Doses above 5 mg/day were administered in two divided doses.
The primary efficacy measure was the percent reduction in the weekly frequency of drop seizures (atonic, tonic, or myoclonic), also known as drop attacks, from the 4-week baseline period to 12-week maintenance period.
The pre-dosing baseline mean weekly drop seizure frequency was 98, 100, 61, and 105 for the placebo, low-, medium-, and high-dose groups, respectively. Figure 1 presents the mean percent reduction in weekly drop seizures from this baseline. All dose groups of ONFI were statistically superior (p≤0.05) to the placebo group. This effect appeared to be dose dependent.
Figure 1. Mean Percent Reduction from Baseline in Weekly Drop Seizure Frequency (Study 1)
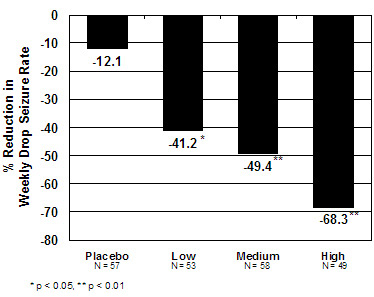
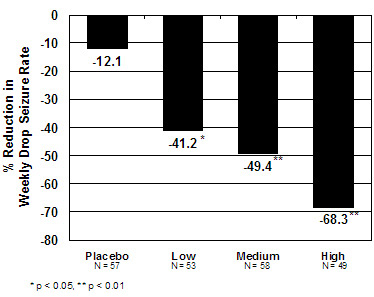
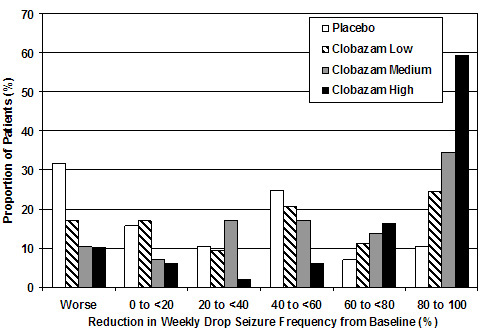
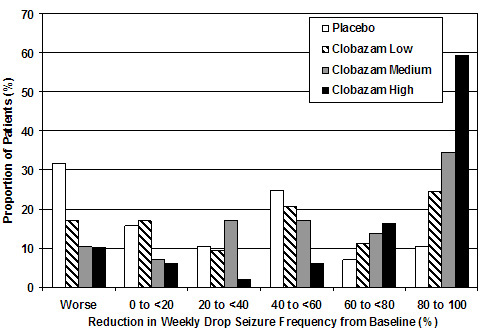
Figure 2 shows changes from baseline in weekly drop seizure frequency by category for patients treated with ONFI and placebo in Study 1. Patients in whom the seizure frequency increased are shown at left as "worse." Patients in whom the seizure frequency decreased are shown in five categories.
Figure 2. Drop Seizure Response by Category for ONFI and Placebo (Study 1)
There was no evidence that tolerance to the therapeutic effect of ONFI developed during the 3-month maintenance period.
Study 2
Study 2 (N=68) was a randomized, double-blind comparison study of high- and low-dose ONFI, consisting of a 4-week baseline period followed by a 3-week titration period and 4-week maintenance period. Patients age 2-25 years with a current or prior diagnosis of LGS were stratified by weight, then randomized to either a low or high dose of ONFI, and then entered a 3-week titration period.
Study 2 (N=68) was a randomized, double-blind comparison study of high- and low-dose ONFI, consisting of a 4-week baseline period followed by a 3-week titration period and 4-week maintenance period. Patients age 2-25 years with a current or prior diagnosis of LGS were stratified by weight, then randomized to either a low or high dose of ONFI, and then entered a 3-week titration period.
The primary efficacy measure was the percent reduction in the weekly frequency of drop seizures (atonic, tonic, or myoclonic), also known as drop attacks, from the 4-week baseline period to the 4-week maintenance period.
A statistically significantly greater reduction in seizure frequency was observed in the high-dose group compared to the low-dose group (median percent reduction of 93% vs 29%; p<0.05).
8HOW SUPPLIED/STORAGE AND HANDLING
Each ONFI tablet contains 10 mg or 20 mg of clobazam and is a white to off-white, oval tablet with a functional score on one side and either a "1" and "0" or a "2" and "0" debossed on the other side.
NDC 67386-314-01: 10 mg scored tablet, Bottles of 100
ONFI oral suspension is a berry flavored off-white liquid supplied in a bottle with child-resistant closure. The oral suspension is packaged with a dispenser set which contains two calibrated oral dosing syringes and a bottle adapter.
Store and dispense ONFI oral suspension in its original bottle in an upright position. Use within 90 days of first opening the bottle, then discard any remainder.
NDC 67386-313-21: 2.5 mg/mL supplied in a bottle containing 120 mL of suspension.
Store tablets and oral suspension at 20°C to 25°C (68°F to 77°F). See USP controlled room temperature.
9PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (
Risks from Concomitant Use with Opioids
Inform patients and caregivers that potentially fatal additive effects may occur if ONFI is used with opioids and not to use such drugs concomitantly unless supervised by a healthcare provider
Abuse, Misuse, and Addiction
Inform patients that the use of ONFI, even at recommended dosages, exposes users to risks of abuse, misuse, and addiction, which can lead to overdose and death, especially when used in combination with other medications (e.g., opioid analgesics), alcohol, and/or illicit substances. Inform patients about the signs and symptoms of benzodiazepine abuse, misuse, and addiction; to seek medical help if they develop these signs and/or symptoms; and on the proper disposal of unused drug
Withdrawal Reactions
Advise patients or caregivers that abrupt withdrawal of AEDs may increase their risk of seizure. Inform patients that the continued use of ONFI may lead to clinically significant physical dependence and that abrupt discontinuation or rapid dosage reduction of ONFI may precipitate acute withdrawal reactions, which can be life-threatening. Inform patients that in some cases, patients taking benzodiazepines have developed a protracted withdrawal syndrome with withdrawal symptoms lasting weeks to more than 12 months. Instruct patients that discontinuation or dosage reduction of ONFI may require a slow taper
Somnolence or Sedation
Advise patients or caregivers to check with their healthcare provider before ONFI is taken with other CNS depressants such as other benzodiazepines, opioids, tricyclic antidepressants, sedating antihistamines, or alcohol
If applicable, caution patients about operating hazardous machinery, including automobiles, until they are reasonably certain that ONFI does not affect them adversely (e.g., impair judgment, thinking or motor skills).
Hypersensitivity
Inform patients or caregivers that ONFI is contraindicated in patients with a history of hypersensitivity to the drug or its ingredients
Interactions with Hormonal ContraceptivesCounsel women to also use non-hormonal methods of contraception when ONFI is used with hormonal contraceptives and to continue these alternative methods for 28 days after discontinuing ONFI to ensure contraceptive reliability [see Drug Interactions (.
Serious Dermatological ReactionsAdvise patients or caregivers that serious skin reactions have been reported in patients taking ONFI. Serious skin reactions, including SJS/TEN, may need to be treated in a hospital and may be life-threatening. If a skin reaction occurs while taking ONFI, patients or caregivers should consult with healthcare providers immediately [see Warnings and Precautions (.
DRESS/Multiorgan Hypersensitivity
Instruct patients and caregivers that a fever or rash associated with signs of other organ system involvement (e.g., lymphadenopathy, hepatic dysfunction) may be drug-related and should be reported to their healthcare provider immediately. ONFI should be discontinued immediately if a serious hypersensitivity reaction is suspected
Suicidal Thinking and BehaviorCounsel patients, their caregivers, and their families that AEDs, including ONFI, may increase the risk of suicidal thoughts and behavior and advise them of the need to be alert for the emergence or worsening of symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts of self-harm. Patients should report behaviors of concern immediately to healthcare providers [see Warnings and Precautions (.
Pregnancy
Advise pregnant females that the use of ONFI late in pregnancy can result in sedation (respiratory depression, lethargy, hypotonia) and/or withdrawal symptoms (hyperreflexia, irritability, restlessness, tremors, inconsolable crying, and feeding difficulties) in newborns [see Warnings and Precautions (. Instruct patients to notify their healthcare provider if they are pregnant.
Advise pregnant females that the use of ONFI late in pregnancy can result in sedation (respiratory depression, lethargy, hypotonia) and/or withdrawal symptoms (hyperreflexia, irritability, restlessness, tremors, inconsolable crying, and feeding difficulties) in newborns [see Warnings and Precautions (. Instruct patients to notify their healthcare provider if they are pregnant.
Encourage patients to enroll in the North American Antiepileptic Drug (NAAED) Pregnancy Registry if they become pregnant while taking ONFI. The registry is collecting information about the safety of antiepileptic drugs during pregnancy
Lactation
Counsel patients that clobazam, the active ingredient in ONFI, is excreted in breast milk. Instruct patients to notify their healthcare provider if they are breastfeeding or intend to breastfeed. Instruct breastfeeding patients who have been administered ONFI to observe their infants for sedation, poor feeding and poor weight gain, and to seek medical attention if they notice these signs [see Use in Specific Populations (.
Counsel patients that clobazam, the active ingredient in ONFI, is excreted in breast milk. Instruct patients to notify their healthcare provider if they are breastfeeding or intend to breastfeed. Instruct breastfeeding patients who have been administered ONFI to observe their infants for sedation, poor feeding and poor weight gain, and to seek medical attention if they notice these signs [see Use in Specific Populations (.
Tablets manufactured by: Catalent Pharma Solutions, LLC
Oral suspension manufactured by: Rosemont Pharmaceuticals, Ltd.
For: Lundbeck

ONFI is a registered trademark of Lundbeck
10
MEDICATION GUIDEONFI(clobazam)ablets and oral suspension, C-IV
What is the most important information I should know about ONFI?
- ONFI is a benzodiazepine medicine. Taking benzodiazepines with opioid medicines, alcohol, or other central nervous system (CNS) depressants (including street drugs) can cause severe drowsiness, breathing problems (respiratory depression), coma, and death. Get emergency help right away if any of the following happens:
- shallow or slowed breathing
- breathing stops (which may lead to the heart stopping)
- excessive sleepiness (sedation)
Do not drive or operate heavy machinery until you know how taking ONFI with opioids affects you. - Risk of abuse, misuse, and addiction. There is a risk of abuse, misuse, and addiction with benzodiazepines, including ONFI, which can lead to overdose and serious side effects including coma and death.
- Serious side effects including coma and death have happened in people who have abused or misused benzodiazepines, including ONFI. These serious side effects may also include delirium, paranoia, suicidal thoughts or actions, seizures, and difficulty breathing. Call your healthcare provider or go to the nearest hospital emergency room right away if you get any of these serious side effects.
- You can develop an addiction even if you take ONFI as prescribed by your healthcare provider.
- Take ONFI exactly as your healthcare provider prescribed.
- Do not share your ONFI with other people.
- Keep ONFI in a safe place and away from children.
- Physical dependence and withdrawal reactions. ONFI can cause physical dependence and withdrawal reactions.
- Do not suddenly stop taking ONFI. Stopping ONFI suddenly can cause serious and life-threatening side effects, including, unusual movements, responses, or expressions, seizures, sudden and severe mental or nervous system changes, depression, seeing or hearing things that others do not see or hear, an extreme increase in activity or talking, losing touch with reality, and suicidal thoughts or actions. Call your healthcare provider or go to the nearest hospital emergency room right away if you get any of these symptoms.
- Some people who suddenly stop , including, anxiety, trouble remembering, learning, or concentrating, depression, problems sleeping, feeling like insects are crawling under your skin, weakness, shaking, muscle twitching, burning or prickling feeling in your hands, arms, legs or feet, and ringing in your ears.
- Physical dependence is not the same as drug addiction. Your healthcare provider can tell you more about the differences between physical dependence and drug addiction.
- Do not take more ONFI than prescribed or take ONFI for longer than prescribed.
- ONFI can make you sleepy or dizzy and can slow your thinking and motor skills.
- Do not drive, operate heavy machinery, or do other dangerous activities until you know how ONFI affects you.
- Do not drink alcohol or take other drugs that may make you sleepy or dizzy while taking ONFI without first talking to your healthcare provider. When taken with alcohol or drugs that cause sleepiness or dizziness, ONFI may make your sleepiness or dizziness much worse.
- Serious skin reactions have been seen when ONFI is taken with other medicines and may require stopping its use. Do not stop taking ONFI without first talking to your healthcare provider.
- A serious skin reaction can happen at any time during your treatment with ONFI, but is more likely to happen within the first 8 weeks of treatment. These skin reactions may need to be treated right away.
- Call your healthcare provider immediately if you have skin blisters, rash, sores in mouth, hives or any other allergic reaction.
- A serious allergic reaction that may affect your skin or other parts of your body such as your liver, kidneys, heart, or blood cells. This allergic reaction can be life-threatening and can cause death, particularly if it is not treated as early as possible. Call your healthcare provider right away if you have:
- a skin rash
- fever or swollen glands that do not go away
- swelling of your face
- shortness of breath
- dark urine
- yellowing of the skin or whites of the eyes
- Like other antiepileptic medicines, ONFI may cause suicidal thoughts or actions in a very small number of people, about 1 in 500.
Call your healthcare provider right away if you have any of these symptoms, especially if they are new, worse, or worry you:
- thoughts about suicide or dying
- attempts to commit suicide
- new or worse depression
- new or worse anxiety or irritability
- feeling agitated or restless
- an extreme increase in activity and talking (mania)
- trouble sleeping (insomnia)
- new or worse panic attacks
- acting aggressive, being angry or violent
- acting on dangerous impulses
- other unusual changes in behavior or mood
How can I watch for early symptoms of suicidal thoughts and actions?
- Pay attention to any changes, especially sudden changes, in mood, behaviors, thoughts, or feelings.
- Keep all follow-up visits with your healthcare provider as scheduled.
Call your healthcare provider between visits as needed, especially if you are worried about symptoms.
Stopping a seizure medicine suddenly in a patient who has epilepsy can cause seizures that will not stop (status epilepticus).
Suicidal thoughts or actions can be caused by things other than medicines. If you have suicidal thoughts or actions, your healthcare provider may check for other causes.
What is ONFI?
- ONFI is a prescription medicine used along with other medicines to treat seizures associated with Lennox-Gastaut syndrome in people 2 years of age or older.
- ONFI is a federally controlled substance (C-IV) because it Keep ONFI in a safe place to prevent misuse and abuse. Selling or giving away ONFI may harm others, and is against the law. Tell your healthcare provider if you have ever abused or been dependent on alcohol, prescription medicines, or street drugs.
It is not known if ONFI is safe and effective in children less than 2 years old.
Do not take ONFI if you:
- are allergic to clobazam or any of the ingredients in ONFI. See the end of this Medication Guide for a complete list of ingredients in ONFI.
Before you take ONFI, tell your healthcare provider about all your medical conditions, including if you:
- have liver or kidney problems
- have lung problems (respiratory disease)
- have or have had depression, mood problems, or suicidal thoughts or behavior
- use birth control medicine. ONFI may cause your birth control medicine to be less effective. Talk to your healthcare provider about the best birth control method to use.
- are pregnant or plan to become pregnant.
- are breastfeeding or plan to breastfeed. ONFI can pass into breast milk.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Taking ONFI with certain other medicines can cause side effects or affect how well ONFI or the other medicines work. Do not start or stop other medicines without talking to your healthcare provider.
How should I take ONFI?
- Take ONFI exactly as your healthcare provider tells you to take it.
- Your healthcare provider will tell you how much ONFI to take and when to take it.
- ONFI tablets can be taken whole, broken in half along the score, or crushed and mixed in applesauce.
- ONFI tablets and oral suspension can be taken with or without food.
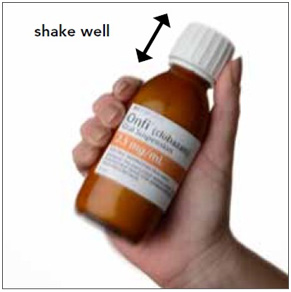
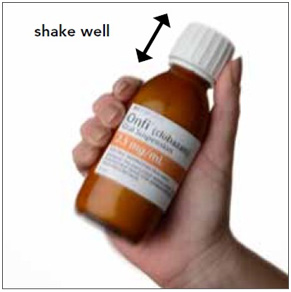
- Shake the bottle of ONFI oral suspension well right before you take each dose.
- Measure your dose of ONFI oral suspension using the bottle adapter and dosing syringes that come with your ONFI oral suspension.
- Read the
- Your healthcare provider may change your dose if needed. Do not change your dose of ONFI without talking to your healthcare provider.
- Do not stop taking ONFI without first talking to your healthcare provider.
- Stopping ONFI suddenly can cause serious problems.
- If you take too much ONFI, call your healthcare provider or go to the nearest hospital emergency room right away.
What should I avoid while taking ONFI?
See
What are the possible side effects of ONFI?
ONFI may cause serious side effects, including: See "What is the most important information I should know about ONFI?"
The most common side effects of ONFI include:
- sleepiness
- drooling
- constipation
- cough
- pain with urination
- fever
- acting aggressive, being angry, or violent
- difficulty sleeping
- slurred speech
- tiredness
- problems with breathing
These are not all the possible side effects of ONFI. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store ONFI?
- Store ONFI tablets and oral suspension at room temperature between 68°F to 77°F (20°C to 25°C).
Tablets
- Keep ONFI tablets in a dry place.
Oral Suspension
- Replace the cap securely after opening.
- Store and dispense the oral suspension in its original bottle in an upright position. Use ONFI oral suspension within 90 days of first opening the bottle.
- After 90 days safely throw away any ONFI oral suspension that has not been used.
- Keep ONFI and all medicines out of the reach of children.
General Information about the safe and effective use of ONFI.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use ONFI for a condition for which it was not prescribed. Do not give ONFI to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about ONFI that is written for health professionals.
What are the ingredients in ONFI?
TabletsActive ingredient: clobazam
Inactive ingredients: modified corn starch, lactose monohydrate, magnesium stearate, silicon dioxide, and talc.
Inactive ingredients: modified corn starch, lactose monohydrate, magnesium stearate, silicon dioxide, and talc.
Oral SuspensionActive ingredient: clobazam
Inactive ingredients: magnesium aluminum silicate, xanthan gum, citric acid monohydrate, disodium hydrogen phosphate dihydrate, simethicone emulsion, polysorbate 80, methylparaben, propylparaben, propylene glycol, sucralose, maltitol solution, berry flavor, purified water.
Inactive ingredients: magnesium aluminum silicate, xanthan gum, citric acid monohydrate, disodium hydrogen phosphate dihydrate, simethicone emulsion, polysorbate 80, methylparaben, propylparaben, propylene glycol, sucralose, maltitol solution, berry flavor, purified water.
Marketed by: Lundbeck, Deerfield, IL 60015, U.S.A.
ONFI is a registered trademark of Lundbeck
For more information about ONFI, go to

This Medication Guide has been approved by the U.S. Food and Drug Administration Revised: 3/2024
Instructions for Use
ONFI(clobazam)Oral Suspension, CIV
Read this Instructions for Use before using ONFI oral suspension and each time you get a refill. There may be new information. This leaflet does not take the place of talking with your healthcare provider about your medical condition or treatment.
Prepare ONFI Oral Suspension DoseYou will need the following supplies: See Figure A
- ONFI oral suspension bottle
- Bottle adapter
- Oral dosing syringe (2 dosing syringes are included in the ONFI oral suspension box).
- Use only 1 syringe to take your dose of ONFI oral suspension. If you lose or damage the syringe, or cannot read the markings, use the other syringe.
Figure A


Step 1. Remove the ONFI oral suspension bottle, bottle adapter, and 1 syringe from the box.
Step 2. Shake the bottle well before each use. See Figure B
Figure B
Step 3. Uncap the bottle and firmly insert the bottle adapter into the bottle until the adapter top is even with the bottle top. See Figure C
Figure C
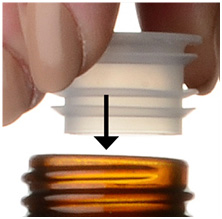
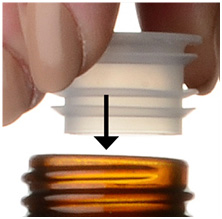
Once the bottle adapter is in place, it should not be removed.
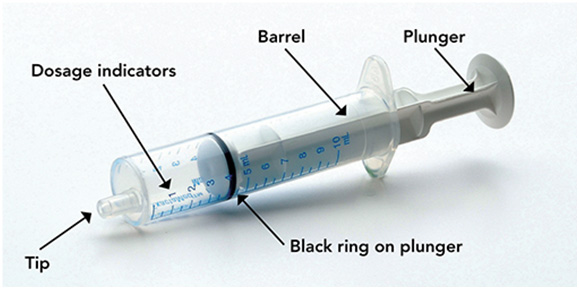
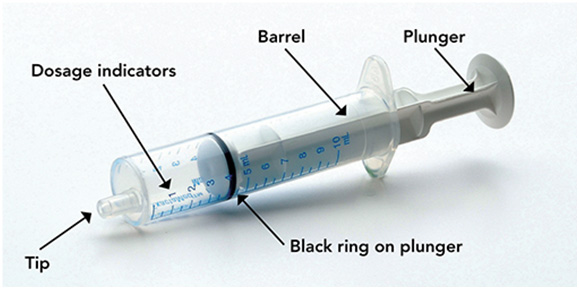
Step 4. Check your dose in milliliters (mL) as prescribed by your healthcare provider. Find this number on the syringe. Do not take more than the prescribed total dose in 1 day. See Figure D
Figure D
Step 5. Push the plunger all the way down and then insert the syringe into the upright bottle through the opening in the bottle adapter. See Figure E
Figure E
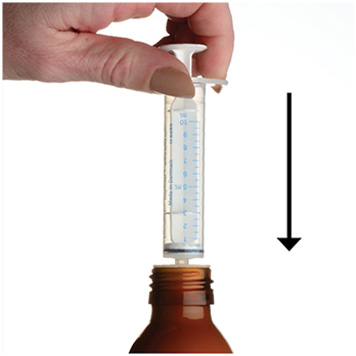
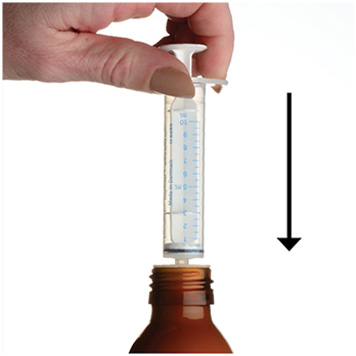
Step 6. With the syringe in place, turn the bottle upside down. Pull the plunger to the number of mLs needed (the amount of liquid medicine in Step 4). See Figure F
Figure F
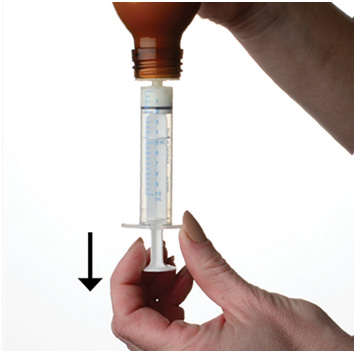
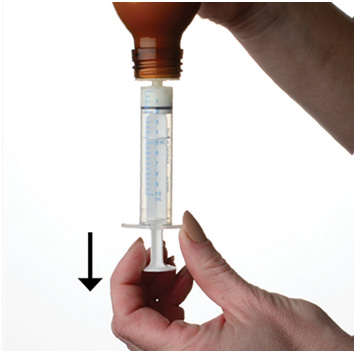
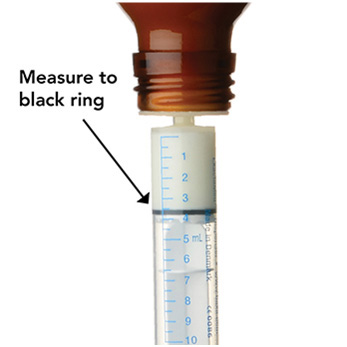
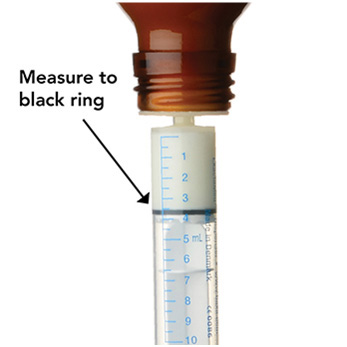
Measure the mLs of medicine using the black ring on the white plunger.
Figure G
Step 7. Remove the syringe from the bottle adapter. Slowly squirt ONFI oral suspension directly into the corner of your mouth or your child's mouth until all of the liquid medicine in the syringe is given. See Figure H
Figure H


Step 8. Cap the bottle tightly with the adapter in place. If the cap does not fit securely, check to see if the adapter is fully inserted. See Figure I
- Store and dispense ONFI oral suspension in its original bottle in an upright position at 68°F to 77°F (20°C to 25°C).
- Use ONFI oral suspension within 90 days of first opening bottle.
- After 90 days safely throw away any ONFI oral suspension that has not been used.
Figure I


Step 9. Wash the oral syringe after each use.
- To clean the oral syringe, take apart by removing the plunger completely. Pull plunger straight out of the barrel.
- The barrel and plunger can be washed with soap and water, rinsed, and allowed to dry.
- Do not wash the oral syringe in the dishwasher.
This Instruction for Use has been approved by the U.S. Food and Drug Administration.
Marketed by: Lundbeck, Deerfield, IL 60015, U.S.A.

ONFI is a registered trademark of Lundbeck
12/2016