Brand Name
Faslodex
Generic Name
Fulvestrant
View Brand Information FDA approval date: November 01, 2010
Classification: Estrogen Receptor Antagonist
Form: Injection
What is Faslodex (Fulvestrant)?
Monotherapy Fulvestrant injection is indicated for the treatment of: Hormone receptor -positive, human epidermal growth factor receptor 2 -negative advanced breast cancer in postmenopausal women not previously treated with endocrine therapy, or HR-positive advanced breast cancer in postmenopausal women with disease progression following endocrine therapy. Combination Therapy Fulvestrant injection is indicated for the treatment of: HR-positive, HER2-negative advanced or metastatic breast cancer in postmenopausal women in combination with ribociclib as initial endocrine based therapy or following disease progression on endocrine therapy. HR-positive, HER2-negative advanced or metastatic breast cancer in combination with palbociclib or abemaciclib in women with disease progression after endocrine therapy. Fulvestrant injection is an estrogen receptor antagonist indicated for the treatment of: Hormone receptor -positive, human epidermal growth factor receptor 2 -negative advanced breast cancer in postmenopausal women not previously treated with endocrine therapy. HR-positive advanced breast cancer in postmenopausal women with disease progression following endocrine therapy. HR-positive, HER2-negative advanced or metastatic breast cancer in postmenopausal women in combination with ribociclib, as initial endocrine based therapy or following disease progression on endocrine therapy. HR-positive, HER2-negative advanced or metastatic breast cancer in combination with palbociclib or abemaciclib in women with disease progression after endocrine therapy.
Approved To Treat
Top Global Experts
There are no experts for this drug
Save this treatment for later
Not sure about your diagnosis?
Related Clinical Trials
There is no clinical trials being done for this treatment
Related Latest Advances
There is no latest advances for this treatment
Brand Information
FASLODEX (Fulvestrant)
1INDICATIONS AND USAGE
Monotherapy
FASLODEX is indicated for the treatment of:
- Hormone receptor (HR)-positive, human epidermal growth factor receptor 2 (HER2)-negative advanced breast cancer in postmenopausal women not previously treated with endocrine therapy, or
- HR-positive advanced breast cancer in postmenopausal women with disease progression following endocrine therapy.
Combination Therapy
FASLODEX is indicated for the treatment of:
- HR-positive, HER2-negative advanced or metastatic breast cancer in postmenopausal women in combination with ribociclib as initial endocrine based therapy or following disease progression on endocrine therapy.
- HR-positive, HER2-negative advanced or metastatic breast cancer in combination with palbociclib or abemaciclib in women with disease progression after endocrine therapy.
2DOSAGE FORMS AND STRENGTHS
FASLODEX, an injection for intramuscular administration, is supplied as 5-mL single-dose prefilled syringes containing 250 mg/5 mL fulvestrant.
3CONTRAINDICATIONS
FASLODEX is contraindicated in patients with a known hypersensitivity to the drug or to any of its components. Hypersensitivity reactions, including urticaria and angioedema, have been reported in association with FASLODEX
4ADVERSE REACTIONS
The following adverse reactions are discussed in more detail in other sections of the labeling:
- Risk of Bleeding
- Increased Exposure in Patients with Hepatic Impairment
- Injection Site Reaction
- Embryo-Fetal Toxicity
4.1Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, the adverse reaction rates observed cannot be directly compared to rates in other trials and may not reflect the rates observed in clinical practice.
Monotherapy
Comparison of FASLODEX 500 mg and FASLODEX 250 mg (CONFIRM)
The following adverse reactions (ARs) were calculated based on the safety analysis of CONFIRM comparing the administration of FASLODEX 500 mg intramuscularly once a month with FASLODEX 250 mg intramuscularly once a month. The most frequently reported adverse reactions in the FASLODEX 500 mg group were injection site pain (11.6% of patients), nausea (9.7% of patients), and bone pain (9.4% of patients); the most frequently reported adverse reactions in the FASLODEX 250 mg group were nausea (13.6% of patients), back pain (10.7% of patients), and injection site pain (9.1% of patients).
Table 1 lists adverse reactions reported with an incidence of 5% or greater, regardless of assessed causality, from CONFIRM.
In the pooled safety population (N=1127) from clinical trials comparing FASLODEX 500 mg to FASLODEX 250 mg, post-baseline increases of ≥1 CTC grade in either AST, ALT, or alkaline phosphatase were observed in >15% of patients receiving FASLODEX. Grade 3-4 increases were observed in 1-2% of patients. The incidence and severity of increased hepatic enzymes (ALT, AST, ALP) did not differ between the 250 mg and the 500 mg FASLODEX arms.
Comparison of FASLODEX 500 mg and Anastrozole 1 mg (FALCON)
The safety of FASLODEX 500 mg versus anastrozole 1 mg was evaluated in FALCON. The data described below reflect exposure to FASLODEX in 228 out of 460 patients with HR-positive advanced breast cancer in postmenopausal women not previously treated with endocrine therapy who received at least one (1) dose of treatment in FALCON.
Permanent discontinuation associated with an adverse reaction occurred in 4 of 228 (1.8%) patients receiving FASLODEX and in 3 of 232 (1.3%) patients receiving anastrozole. Adverse reactions leading to discontinuation for those patients receiving FASLODEX included drug hypersensitivity (0.9%), injection site hypersensitivity (0.4%), and elevated liver enzymes (0.4%).
The most common adverse reactions (≥10%) of any grade reported in patients in the FASLODEX arm were arthralgia, hot flash, fatigue, and nausea.
Adverse reactions reported in patients who received FASLODEX in FALCON at an incidence of ≥5% in either treatment arm are listed in Table 2, and laboratory abnormalities are listed in Table 3.
Comparison of FASLODEX 250 mg and Anastrozole 1 mg in Combined Trials (Studies 0020 and 0021)
The most commonly reported adverse reactions in the FASLODEX and anastrozole treatment groups were gastrointestinal symptoms (including nausea, vomiting, constipation, diarrhea, and abdominal pain), headache, back pain, vasodilatation (hot flashes), and pharyngitis.
Injection site reactions with mild transient pain and inflammation were seen with FASLODEX and occurred in 7% of patients given the single 5 mL injection (Study 0020) and in 27% of patients given the 2 x 2.5 mL injections (Study 0021) in the two clinical trials that compared FASLODEX 250 mg and anastrozole 1 mg.
Table 4 lists adverse reactions reported with an incidence of 5% or greater, regardless of assessed causality, from the two controlled clinical trials comparing the administration of FASLODEX 250 mg intramuscularly once a month with anastrozole 1 mg orally once a day.
Combination Therapy
Combination Therapy with Palbociclib (PALOMA-3)
The safety of FASLODEX 500 mg plus palbociclib 125 mg/day versus FASLODEX plus placebo was evaluated in PALOMA-3. The data described below reflect exposure to FASLODEX plus palbociclib in 345 out of 517 patients with HR-positive, HER2-negative advanced or metastatic breast cancer who received at least 1 dose of treatment in PALOMA-3. The median duration of treatment for FASLODEX plus palbociclib was 10.8 months while the median duration of treatment for FASLODEX plus placebo arm was 4.8 months.
No dose reduction was allowed for FASLODEX in PALOMA-3. Dose reductions of palbociclib due to an adverse reaction of any grade occurred in 36% of patients receiving FASLODEX plus palbociclib.
Permanent discontinuation associated with an adverse reaction occurred in 19 of 345 (6%) patients receiving FASLODEX plus palbociclib, and in 6 of 172 (3%) patients receiving FASLODEX plus placebo. Adverse reactions leading to discontinuation for those patients receiving FASLODEX plus palbociclib included fatigue (0.6%), infections (0.6%), and thrombocytopenia (0.6%).
The most common adverse reactions (≥10%) of any grade reported in patients in the FASLODEX plus palbociclib arm by descending frequency were neutropenia, leukopenia, infections, fatigue, nausea, anemia, stomatitis, diarrhea, thrombocytopenia, vomiting, alopecia, rash, decreased appetite, and pyrexia.
The most frequently reported Grade ≥3 adverse reactions (≥5%) in patients receiving FASLODEX plus palbociclib in descending frequency were neutropenia and leukopenia.
Adverse reactions (≥10%) reported in patients who received FASLODEX plus palbociclib or FASLODEX plus placebo in PALOMA-3 are listed in Table 5, and laboratory abnormalities are listed in Table 6.
Additional adverse reactions occurring at an overall incidence of <10.0% of patients receiving FASLODEX plus palbociclib in PALOMA-3 included asthenia (7.5%), aspartate aminotransferase increased (7.5%), dysgeusia (6.7%), epistaxis (6.7%), lacrimation increased (6.4%), dry skin (6.1%), alanine aminotransferase increased (5.8%), vision blurred (5.8%), dry eye (3.8%), and febrile neutropenia (0.9%).
N=number of patients; WBC=white blood cells.
Combination Therapy with Abemaciclib (MONARCH 2)
The safety of FASLODEX (500 mg) plus abemaciclib (150 mg twice daily) versus FASLODEX plus placebo was evaluated in MONARCH 2. The data described below reflect exposure to FASLODEX in 664 patients with HR-positive, HER2-negative advanced breast cancer who received at least one dose of FASLODEX plus abemaciclib or placebo in MONARCH 2.
Median duration of treatment was 12 months for patients receiving FASLODEX plus abemaciclib and 8 months for patients receiving FASLODEX plus placebo.
Dose reductions due to an adverse reaction occurred in 43% of patients receiving FASLODEX plus abemaciclib. Adverse reactions leading to dose reductions ≥5% of patients were diarrhea and neutropenia. Abemaciclib dose reduction due to diarrhea of any grade occurred in 19% of patients receiving FASLODEX plus abemaciclib compared to 0.4% of patients receiving FASLODEX plus placebo. Abemaciclib dose reductions due to neutropenia of any grade occurred in 10% of patients receiving FASLODEX plus abemaciclib compared to no patients receiving FASLODEX plus placebo.
Permanent study treatment discontinuation due to an adverse event was reported in 9% of patients receiving FASLODEX plus abemaciclib and in 3% of patients receiving FASLODEX plus placebo. Adverse reactions leading to permanent discontinuation for patients receiving FASLODEX plus abemaciclib were infection (2%), diarrhea (1%), hepatotoxicity (1%), fatigue (0.7%), nausea (0.2%), abdominal pain (0.2%), acute kidney injury (0.2%), and cerebral infarction (0.2%).
Deaths during treatment or during the 30-day follow up, regardless of causality, were reported in 18 cases (4%) of FASLODEX plus abemaciclib treated patients versus 10 cases (5%) of FASLODEX plus placebo treated patients. Causes of death for patients receiving FASLODEX plus abemaciclib included: 7 (2%) patient deaths due to underlying disease, 4 (0.9%) due to sepsis, 2 (0.5%) due to pneumonitis, 2 (0.5%) due to hepatotoxicity, and one (0.2%) due to cerebral infarction.
The most common adverse reactions reported (≥20%) in the FASLODEX plus abemaciclib arm were diarrhea, fatigue, neutropenia, nausea, infections, abdominal pain, anemia, leukopenia, decreased appetite, vomiting, and headache (Table 7). The most frequently reported (≥5%) Grade 3 or 4 adverse reactions were neutropenia, diarrhea, leukopenia, anemia, and infections.
Additional adverse reactions in MONARCH 2 include venous thromboembolic events (deep vein thrombosis, pulmonary embolism, cerebral venous sinus thrombosis, subclavian vein thrombosis, axillary vein thrombosis, and DVT inferior vena cava), which were reported in 5% of patients treated with FASLODEX plus abemaciclib as compared to 0.9% of patients treated with FASLODEX plus placebo.
Combination Therapy with Ribociclib (MONALEESA-3)
The safety of FASLODEX 500 mg plus ribociclib 600 mg versus FASLODEX plus placebo was evaluated in MONALEESA-3. The data described below reflect exposure to FASLODEX plus ribociclib in 483 out of 724 postmenopausal patients with HR-positive, HER2-negative advanced or metastatic breast cancer for initial endocrine based therapy or after disease progression on endocrine therapy who received at least one dose of FASLODEX plus ribociclib or placebo in MONALEESA-3. Median duration of treatment was 15.8 months for FASLODEX plus ribociclib and 12 months for FASLODEX plus placebo.
Dose reductions due to adverse reactions occurred in 32% of patients receiving FASLODEX plus ribociclib and in 3% of patients receiving FASLODEX plus placebo. Among patients receiving FASLODEX plus ribociclib, 8% were reported to have permanently discontinued both FASLODEX plus ribociclib, and 9% were reported to have discontinued ribociclib alone due to ARs. Among patients receiving FASLODEX plus placebo, 4% were reported to have permanently discontinued both FASLODEX and placebo and 2% were reported to have discontinued placebo alone due to ARs.
Adverse reactions leading to treatment discontinuation of FASLODEX plus ribociclib (as compared to FASLODEX plus placebo) were ALT increased (5% vs. 0%), AST increased (3% vs. 0.6%), and vomiting (1% vs. 0%).
The most common adverse reactions (reported at a frequency ≥20% on the FASLODEX plus ribociclib arm and ≥2% higher than FASLODEX plus placebo) were neutropenia, infections, leukopenia, cough, nausea, diarrhea, vomiting, constipation, pruritus, and rash. The most frequently reported Grade 3/4 adverse reactions (reported at a frequency ≥5%) in patients receiving FASLODEX plus ribociclib in descending frequency were neutropenia, leukopenia, infections, and abnormal liver function tests.
Adverse reactions and laboratory abnormalities occurring in patients in MONALEESA-3 are listed in Table 9 and Table 10, respectively.
Additional adverse reactions in MONALEESA-3 for patients receiving FASLODEX plus ribociclib included asthenia (14%), dyspepsia (10%), thrombocytopenia (9%), dry skin (8%), dysgeusia (7%), electrocardiogram QT prolonged (6%), dry mouth (5%), vertigo (5%), dry eye (5%), lacrimation increased (4%), erythema (4%), hypocalcemia (4%), blood bilirubin increased (1%), and syncope (1%).
4.2Postmarketing Experience
The following adverse reactions have been identified during post-approval use of FASLODEX. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
For FASLODEX 250 mg, other adverse reactions reported as drug-related and seen infrequently (<1%) include thromboembolic phenomena, myalgia, vertigo, leukopenia, and hypersensitivity reactions, including angioedema and urticaria.
Vaginal bleeding has been reported infrequently (<1%), mainly in patients during the first 6 weeks after changing from existing hormonal therapy to treatment with FASLODEX. If bleeding persists, further evaluation should be considered.
Elevation of bilirubin, elevation of gamma GT, hepatitis, and liver failure have been reported infrequently (<1%).
5DRUG INTERACTIONS
There are no known drug-drug interactions. Although, fulvestrant is metabolized by CYP 3A4
6OVERDOSAGE
Human experience of overdose with FASLODEX is limited. There are isolated reports of overdose with FASLODEX in humans. No adverse reactions were seen in healthy male and female volunteers who received intravenous fulvestrant, which resulted in peak plasma concentrations at the end of the infusion, that were approximately 10 to 15 times those seen after intramuscular injection. The potential toxicity of fulvestrant at these or higher concentrations in cancer patients who may have additional comorbidities is unknown. There is no specific treatment in the event of fulvestrant overdose, and symptoms of overdose are not established. In the event of an overdose, healthcare practitioners should follow general supportive measures and should treat symptomatically.
7DESCRIPTION
FASLODEX
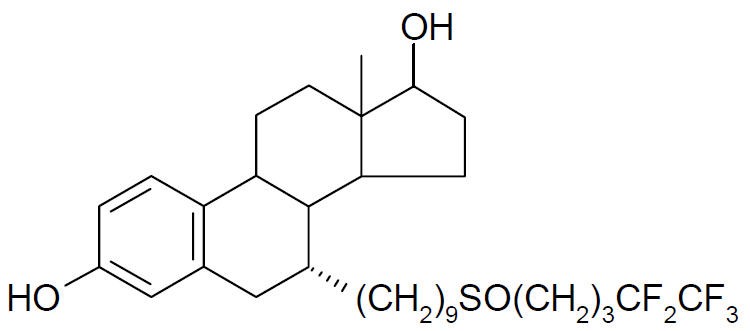
Fulvestrant is a white powder with a molecular weight of 606.77. The solution for injection is a clear, colorless to yellow, viscous liquid.
Each injection contains as inactive ingredients: 10% w/v Alcohol, USP, 10% w/v Benzyl Alcohol, NF, and 15% w/v Benzyl Benzoate, USP, as co-solvents, and made up to 100% w/v with Castor Oil, USP as a co-solvent and release rate modifier.
8CLINICAL STUDIES
The efficacy of FASLODEX 500 mg versus FASLODEX 250 mg was compared in CONFIRM. The efficacy of FASLODEX 250 mg was compared to 1 mg anastrozole in Studies 0020 and 0021. The efficacy of FASLODEX 500 mg was compared to 1 mg anastrozole in FALCON. The efficacy of FASLODEX 500 mg in combination with palbociclib 125 mg was compared to FASLODEX 500 mg plus placebo in PALOMA-3. The efficacy of FASLODEX 500 mg in combination with abemaciclib 150 mg was compared to FASLODEX 500 mg plus placebo in MONARCH 2. The efficacy of FASLODEX 500 mg in combination with ribociclib 600 mg was compared to FASLODEX 500 mg plus placebo in MONALEESA-3.
Monotherapy
Comparison of FASLODEX 500 mg and FASLODEX 250 mg (CONFIRM)
A randomized, double-blind, controlled clinical trial (CONFIRM, NCT00099437) was completed in 736 postmenopausal women with advanced breast cancer who had disease recurrence on or after adjuvant endocrine therapy or progression following endocrine therapy for advanced disease. This trial compared the efficacy and safety of FASLODEX 500 mg (n=362) with FASLODEX 250 mg (n=374).
FASLODEX 500 mg was administered as two 5 mL injections each containing FASLODEX 250 mg/5 mL, one in each buttock, on Days 1, 15, 29, and every 28 (+/- 3) days thereafter. FASLODEX 250 mg was administered as two 5 mL injections (one containing FASLODEX 250 mg/5 mL injection plus one placebo injection), one in each buttock, on Days 1, 15 (2 placebo injections only), 29, and every 28 (+/- 3) days thereafter.
The median age of study participants was 61 years. All patients had ER+ advanced breast cancer. Approximately 30% of subjects had no measurable disease. Approximately 55% of patients had visceral disease.
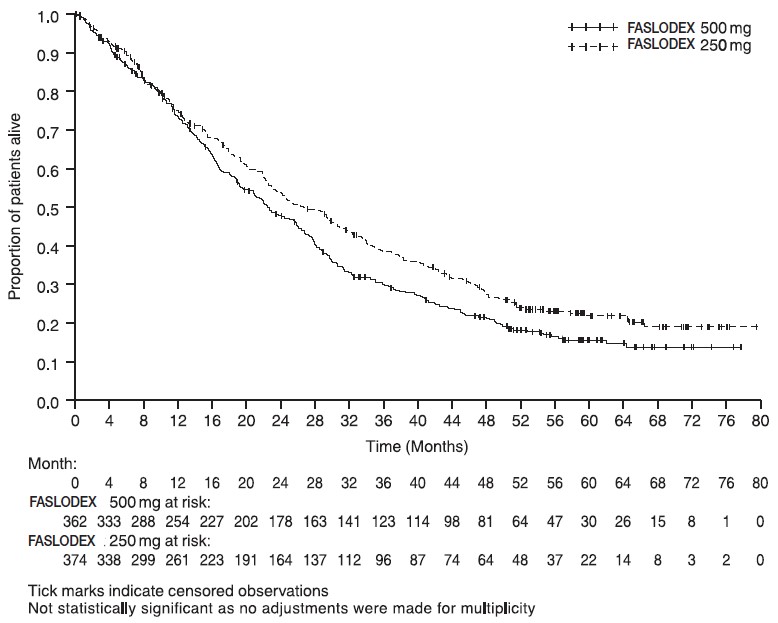
Results of CONFIRM are summarized in Table 12. The efficacy of FASLODEX 500 mg was compared to that of FASLODEX 250 mg. Figure 6 shows a Kaplan-Meier plot of the Progression Free Survival (PFS) data after a minimum follow-up duration of 18 months demonstrating statistically significant superiority of FASLODEX 500 mg vs. FASLODEX 250 mg. In the initial Overall Survival (OS) analysis after a minimum follow-up duration of 18 months, there was no statistically significant difference in OS between the two treatment groups. After a minimum follow-up duration of 50 months, an updated OS analysis was performed. Figure 7 shows a Kaplan-Meier plot of the updated OS data.
Figure 6 Kaplan-Meier PFS: CONFIRM ITT Population
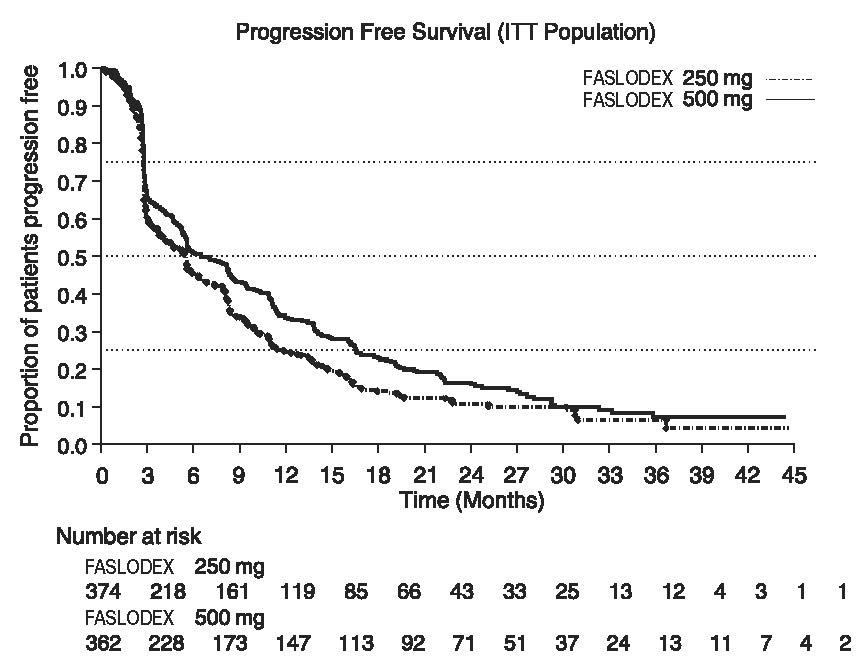
Figure 7 Kaplan-Meier OS (Minimum Follow-up Duration of 50 Months): CONFIRM ITT Population
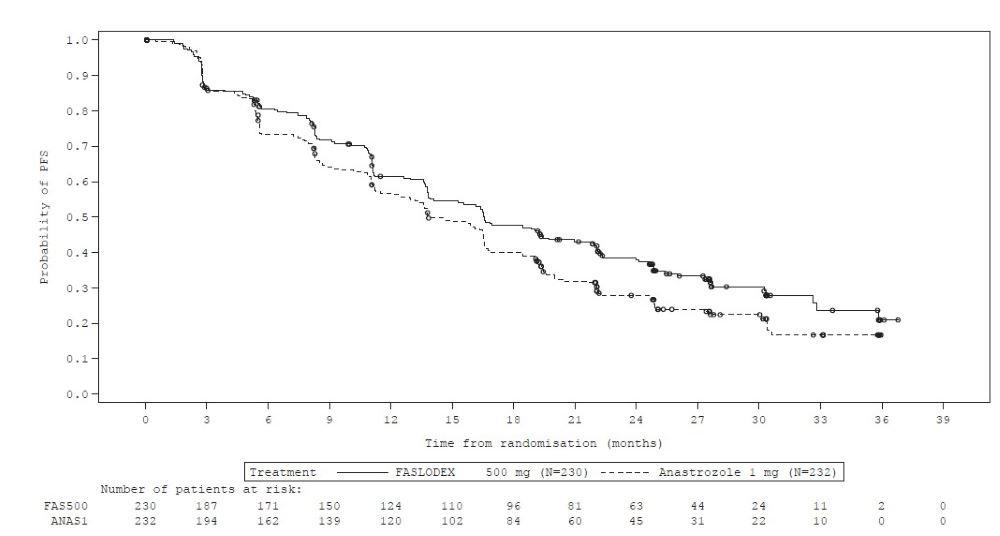
Comparison of FASLODEX 500 mg and Anastrozole 1 mg (FALCON)
A randomized, double-blind, double-dummy, multi-center study (FALCON, NCT01602380) of FASLODEX 500 mg versus anastrozole 1 mg was conducted in postmenopausal women with ER-positive and/or PgR-positive, HER2-negative locally advanced or metastatic breast cancer who had not previously been treated with any hormonal therapy. A total of 462 patients were randomized 1:1 to receive administration of FASLODEX 500 mg as an intramuscular injection on Days 1, 15, 29, and every 28 (+/- 3) days thereafter or daily administration of 1 mg of anastrozole orally. This study compared the efficacy and safety of FASLODEX 500 mg and anastrozole 1 mg.
Randomization was stratified by disease setting (locally advanced or metastatic), use of prior chemotherapy for advanced disease, and presence or absence of measurable disease.
The major efficacy outcome measure of the study was investigator-assessed progression-free survival (PFS) evaluated according to RECIST v.1.1 (Response Evaluation Criteria in Solid Tumors). Key secondary efficacy outcome measures included overall survival (OS), objective response rate (ORR), and duration of response (DoR).
Patients enrolled in this study had a median age of 63 years (range 36-90). The majority of patients (87%) had metastatic disease at baseline. Fifty-five percent (55%) of patients had visceral metastasis at baseline. A total of 17% of patients had received one prior chemotherapy regimen for advanced disease; 84% of patients had measurable disease. Sites of metastases were as follows: musculoskeletal 59%, lymph nodes 50%, respiratory 40%, liver (including gall bladder) 18%.
The efficacy results of FALCON are presented in Table 13 and Figure 8.
Figure 8 Kaplan-Meier Plot of Progression-Free Survival (Investigator Assessment, ITT Population) ─ FALCON
Comparison of FASLODEX 250 mg and Anastrozole 1 mg in Combined Data (Studies 0020 and 0021)
Efficacy of FASLODEX was established by comparison to the selective aromatase inhibitor anastrozole in two randomized, controlled clinical trials (one conducted in North America, Study 0021, NCT00635713; the other predominantly in Europe, Study 0020) in postmenopausal women with locally advanced or metastatic breast cancer. All patients had progressed after previous therapy with an antiestrogen or progestin for breast cancer in the adjuvant or advanced disease setting.
The median age of study participants was 64 years. 81.6% of patients had ER+ and/or PgR+ tumors. Patients with ER-/PgR- or unknown tumors were required to have demonstrated a prior response to endocrine therapy. Sites of metastases occurred as follows: visceral only 18.2%; viscera – liver involvement 23.0%; lung involvement 28.1%; bone only 19.7%; soft tissue only 5.2%; skin and soft tissue 18.7%.
In both trials, eligible patients with measurable and/or evaluable disease were randomized to receive either FASLODEX 250 mg intramuscularly once a month (28 days
Results of the trials, after a minimum follow-up duration of 14.6 months, are summarized in Table 14. The effectiveness of FASLODEX 250 mg was determined by comparing Objective Response Rate (ORR) and Time to Progression (TTP) results to anastrozole 1 mg, the active control. The two studies ruled out (by one-sided 97.7% confidence limit) inferiority of FASLODEX to anastrozole of 6.3% and 1.4% in terms of ORR. There was no statistically significant difference in overall survival (OS) between the two treatment groups after a follow-up duration of 28.2 months in Study 0021 and 24.4 months in Study 0020.
Combination Therapy
Patients with HR-positive, HER2-negative advanced or metastatic breast cancer who have had disease progression on or after prior adjuvant or metastatic endocrine therapy
FASLODEX 500 mg in Combination with Palbociclib 125 mg (PALOMA-3)
PALOMA-3 (NCT-1942135) was an international, randomized, double-blind, parallel group, multi-center study of FASLODEX plus palbociclib versus FASLODEX plus placebo conducted in women with HR-positive, HER2-negative advanced breast cancer, regardless of their menopausal status, whose disease progressed on or after prior endocrine therapy.
A total of 521 pre/postmenopausal women were randomized 2:1 to FASLODEX plus palbociclib or FASLODEX plus placebo and stratified by documented sensitivity to prior hormonal therapy, menopausal status at study entry (pre/peri versus postmenopausal), and presence of visceral metastases. Palbociclib was given orally at a dose of 125 mg daily for 21 consecutive days followed by 7 days off treatment. Fulvestrant 500 mg was administered as two 5 mL injections each containing fulvestrant 250 mg/5 mL, one in each buttock, on Days 1, 15, 29, and every 28 (+/- 3) days thereafter. Pre/perimenopausal women were enrolled in the study and received the LHRH agonist goserelin for at least 4 weeks prior to and for the duration of PALOMA-3.
Patients continued to receive assigned treatment until objective disease progression, symptomatic deterioration, unacceptable toxicity, death, or withdrawal of consent, whichever occurred first. The major efficacy outcome of the study was investigator-assessed PFS evaluated according to RECIST v.1.1.
Patients enrolled in this study had a median age of 57 years (range 29 to 88). The majority of patients on study were White (74%), all patients had an ECOG PS of 0 or 1, and 80% were postmenopausal. All patients had received prior systemic therapy and 75% of patients had received a previous chemotherapy regimen. Twenty-five percent of patients had received no prior therapy in the metastatic disease setting, 60% had visceral metastases, and 23% had bone only disease.
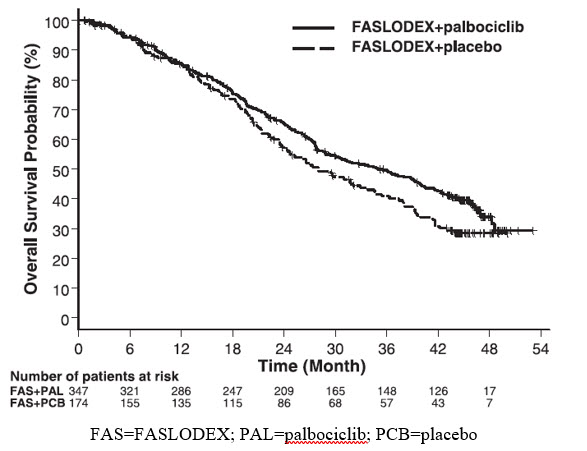
The results from the investigator-assessed PFS and final OS data from PALOMA-3 are summarized in Table 15. The relevant Kaplan-Meier plots are shown in Figures 9 and 10, respectively. Consistent PFS results were observed across patient subgroups of disease site, sensitivity to prior hormonal therapy, and menopausal status. After a median follow-up time of 45 months, the final OS results were not statistically significant.
Figure 9 Kaplan-Meier Plot of Progression-Free Survival (Investigator Assessment, ITT Population) – PALOMA-3
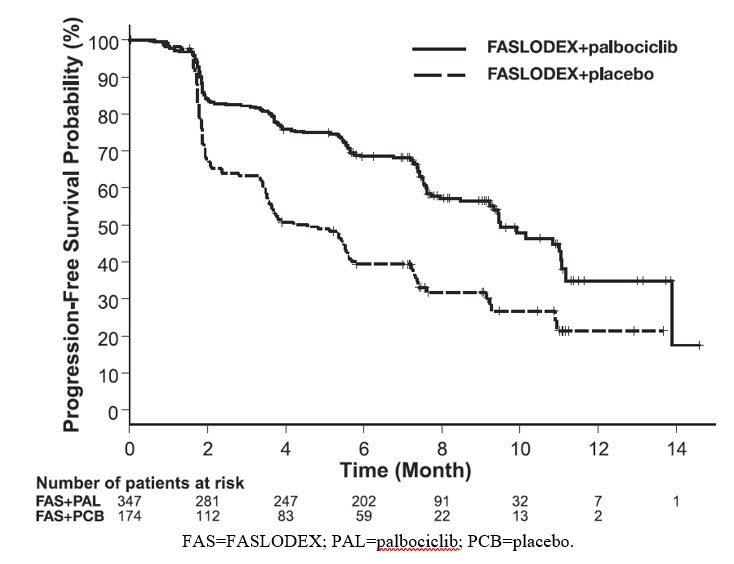
Figure 10 Kaplan-Meier Plot of Overall Survival (ITT Population) ─ PALOMA-3
FASLODEX 500 mg in Combination with Abemaciclib 150 mg (MONARCH 2)
MONARCH 2 (NCT02107703) was a randomized, placebo-controlled, multi-center study conducted in women with HR-positive, HER2-negative metastatic breast cancer with disease progression following endocrine therapy treated with FASLODEX plus abemaciclib versus FASLODEX plus placebo. Randomization was stratified by disease site (visceral, bone only, or other) and by sensitivity to prior endocrine therapy (primary or secondary resistance). A total of 669 patients received intramuscular injection of FASLODEX 500 mg on Days 1 and 15 of cycle 1 and then on Day 1 of cycle 2 and beyond (28-day cycles), plus abemaciclib or placebo orally twice daily. Pre/perimenopausal women were enrolled in the study and received the gonadotropin-releasing hormone agonist goserelin for at least 4 weeks prior to and for the duration of MONARCH 2. Patients remained on continuous treatment until development of progressive disease or unmanageable toxicity.
Patient median age was 60 years (range, 32-91 years), and 37% of patients were older than 65. The majority were White (56%), and 99% of patients had an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1. Twenty percent (20%) of patients had
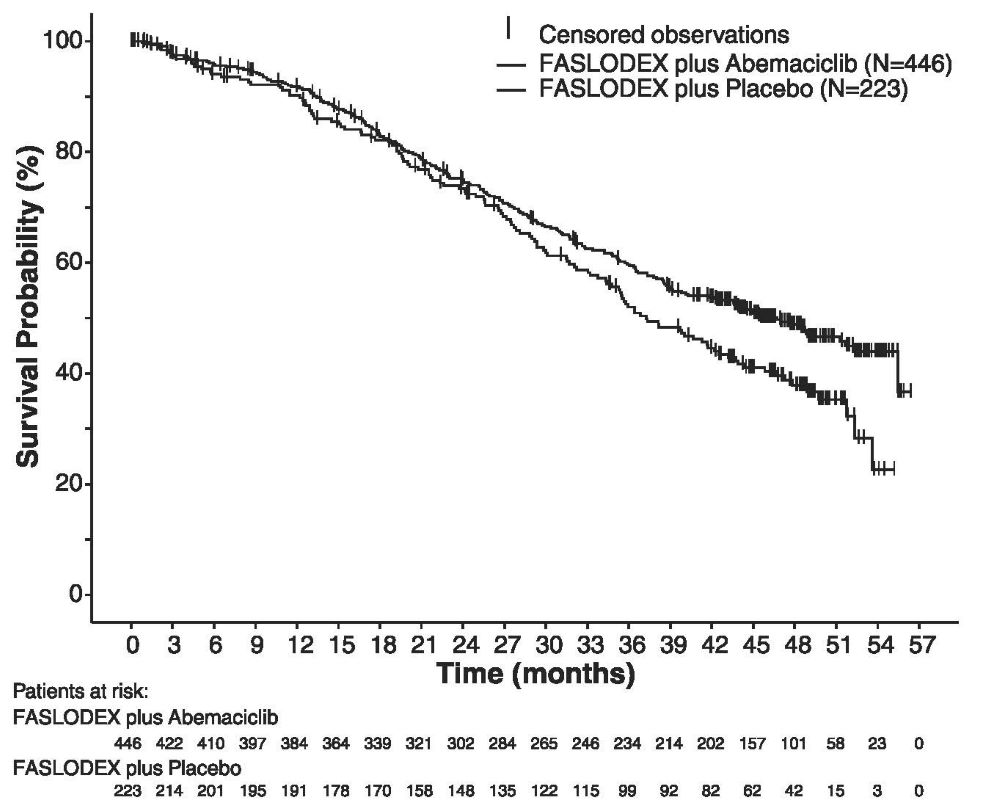
The efficacy results from the MONARCH 2 study are summarized in Table 16, Figure 11, and Figure 12. PFS assessment based on a blinded independent radiologic review was consistent with the investigator assessment. Consistent results were observed across patient stratification subgroups of disease site and endocrine therapy resistance for PFS and OS.
Figure 11 Kaplan-Meier Curves of Progression-Free Survival: FASLODEX Plus Abemaciclib versus FASLODEX plus Placebo (MONARCH 2)
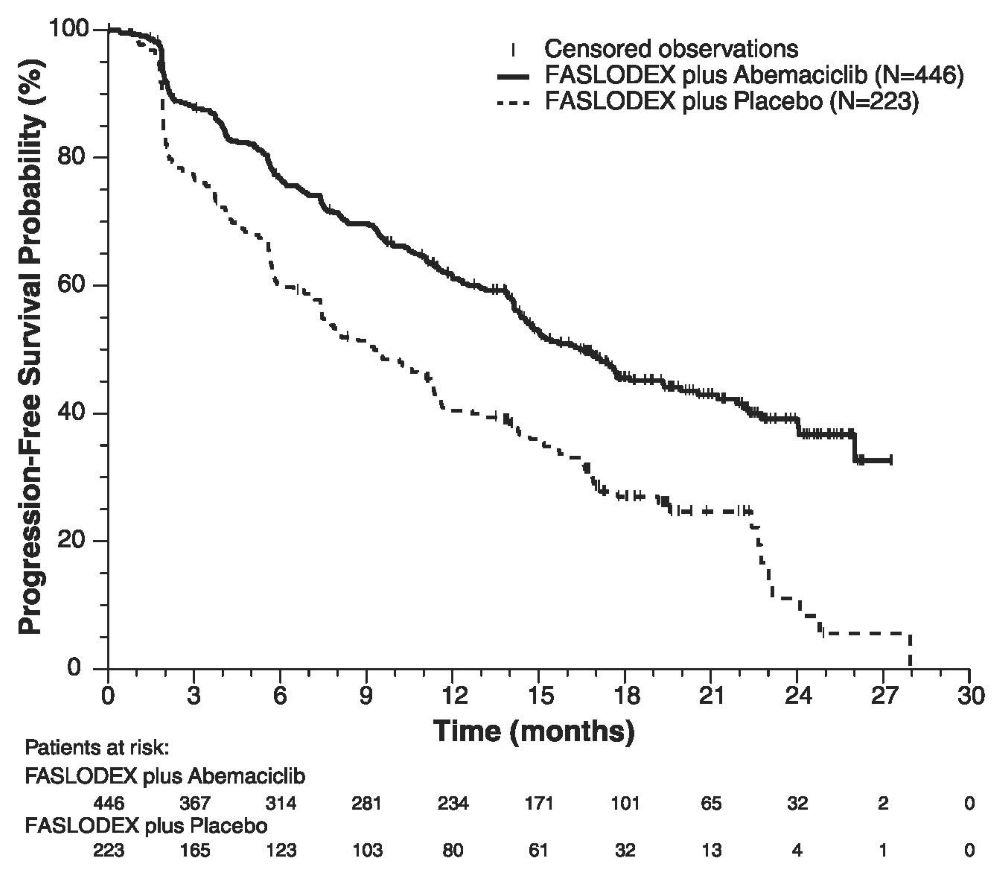
Figure 12 Kaplan-Meier Curves of Overall Survival: FASLODEX plus Abemaciclib versus FASLODEX plus Placebo (MONARCH 2)
Postmenopausal women with HR-positive, HER2-negative advanced or metastatic breast cancer for initial endocrine based therapy or after disease progression on endocrine therapy
FASLODEX 500 mg in Combination with Ribociclib 600 mg (MONALEESA-3)
MONALEESA-3 (NCT 02422615) was a randomized double-blind, placebo-controlled study of FASLODEX plus ribociclib versus FASLODEX plus placebo conducted in postmenopausal women with hormone receptor positive, HER2-negative, advanced breast cancer who have received no or only one line of prior endocrine treatment.
A total of 726 patients were randomized in a 2:1 ratio to receive FASLODEX plus ribociclib or FASLODEX plus placebo and stratified according to the presence of liver and/or lung metastases and prior endocrine therapy for advanced or metastatic disease. Fulvestrant 500 mg was administered intramuscularly on Days 1, 15, 29, and once monthly thereafter, with either ribociclib 600 mg or placebo given orally once daily for 21 consecutive days followed by 7 days off until disease progression or unacceptable toxicity. The major efficacy outcome measure for the study was investigator-assessed progression-free survival (PFS) using Response Evaluation Criteria in Solid Tumors (RECIST) v1.1.
Patients enrolled in this study had a median age of 63 years (range 31 to 89). Of the patients enrolled, 47% were 65 years and older, including 14% age 75 years and older. The patients enrolled were primarily Caucasian (85%), Asian (9%), and Black (0.7%). Nearly all patients (99.7%) had an ECOG performance status of 0 or 1. First- and second-line patients were enrolled in this study (of which 19% had de novo metastatic disease). Forty-three percent (43%) of patients had received chemotherapy in the adjuvant vs. 13% in the neoadjuvant setting and 59% had received endocrine therapy in the adjuvant vs. 1% in the neoadjuvant setting prior to study entry. Twenty-one percent (21%) of patients had bone-only disease and 61% had visceral disease. Demographics and baseline disease characteristics were balanced and comparable between study arms.
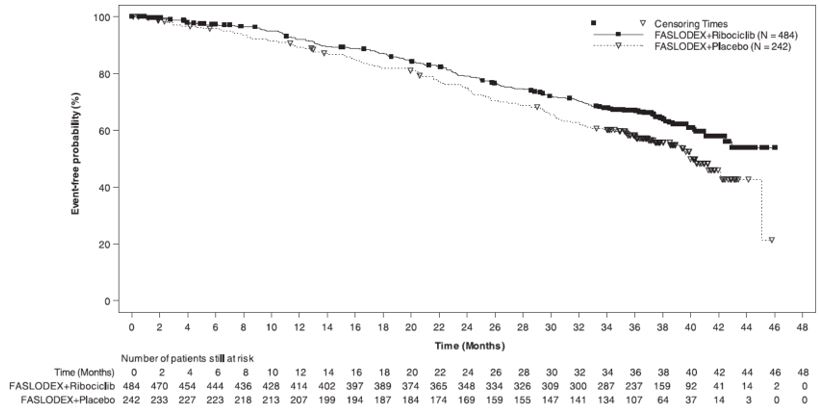
The efficacy results from MONALEESA-3 are summarized in Table 17, Figure 13, and Figure 14. Consistent results were observed in stratification factor subgroups of disease site and prior endocrine treatment for advanced disease.
Figure 13 Kaplan-Meier Progression Free Survival Curves – MONALEESA-3 (Intent-To-Treat Population, Investigator assessment)
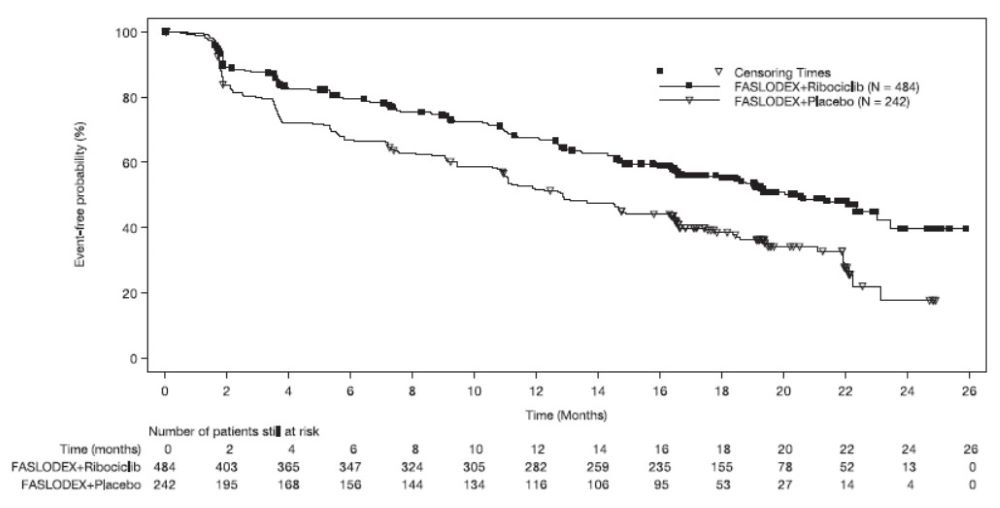
Figure 14 Kaplan-Meier plot of Overall Survival – MONALEESA-3 (Intent -to-Treat Population)
9HOW SUPPLIED/STORAGE AND HANDLING
FASLODEX is supplied as two 5 mL clear neutral glass (Type 1) barrels, each containing 250 mg/5 mL of FASLODEX solution for intramuscular injection and fitted with a tamper evident closure.
NDC 0310–0720–10
The single-dose prefilled syringes are presented in a tray with polystyrene plunger rod and safety needles (SafetyGlide™) for connection to the barrel.
Discard each syringe after use. If a patient dose requires only one syringe, unused syringe should be stored as directed below.
Storage:
REFRIGERATE, 2°-8°C (36°-46°F).
10PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Monotherapy
Risk of Bleeding:
- Because FASLODEX is administered intramuscularly, it should be used with caution in patients with bleeding disorders, decreased platelet count, or in patients receiving anticoagulants (for example, warfarin)
Embryo-Fetal Toxicity:
- Advise females of reproductive potential of the potential risk to a fetus and to use effective contraception during treatment with FASLODEX and for one year after the last dose. Advise females to inform their healthcare provider of a known or suspected pregnancy
Lactation:
- Advise women not to breastfeed during treatment with FASLODEX and for one year after the last dose
Combination Therapy
When FASLODEX is used in combination with palbociclib, abemaciclib, or ribociclib, refer to the respective Full Prescribing Information for Patient Counseling Information.
Distributed by:
AstraZeneca Pharmaceuticals LP
Wilmington, DE 19850
FASLODEX is a registered trademark of the AstraZeneca group of companies
©AstraZeneca 2020
11Package/Label Display Panel – 250 mg/5 mL (50 mg/mL)