RopivacaIne
What is Naropin (RopivacaIne)?
Undergoing surgery or managing severe pain after an injury can be overwhelming, physically and emotionally. The fear of pain often adds anxiety to what is already a stressful experience. Naropin (ropivacaine) helps make this process more comfortable and controlled by providing reliable, long-lasting pain relief.
Naropin is a local anesthetic, meaning it temporarily blocks nerve signals in specific parts of the body to prevent pain during or after medical procedures. It belongs to the amide-type anesthetic drug class, similar to medications such as lidocaine and bupivacaine. Naropin is commonly used by anesthesiologists during surgeries, labor, or diagnostic procedures, as well as for postoperative pain management.
Since its approval by the U.S. Food and Drug Administration (FDA), Naropin has become a widely trusted option because it provides effective anesthesia with a lower risk of certain side effects compared to older local anesthetics. Its precision and safety profile make it a preferred choice in modern pain management and regional anesthesia.
What does Naropin do?
Naropin is used to numb specific areas of the body so that patients do not feel pain during surgical procedures, childbirth, or other medical interventions. It may also be used to control pain after surgery or injury, especially when given through a continuous infusion near the nerves that sense pain.
The drug is typically used in:
- Regional anesthesia (blocking sensation in a larger part of the body, such as the lower half during childbirth or leg surgery)
- Local anesthesia (numbing a small, specific area for minor procedures)
- Postoperative pain control, where Naropin can be administered through a catheter for continuous relief
Patients who receive Naropin usually remain awake but comfortable during the procedure, without feeling pain in the targeted area. Many report smoother recoveries with fewer complications such as drowsiness or nausea, which can occur with general anesthesia.
Clinical research supports Naropin’s effectiveness and safety, showing that it provides pain relief comparable to other local anesthetics but with a lower risk of heart and nervous system toxicity (NIH, 2024). This makes it particularly valuable in patients requiring precise, controlled anesthesia over longer periods.
How does Naropin work?
Naropin works by blocking the transmission of pain signals along the nerves. Normally, when you experience pain, your nerves send electrical messages to the brain through sodium channels in nerve cell membranes. Ropivacaine, the active ingredient in Naropin, blocks these sodium channels, preventing nerve cells from transmitting those signals.
As a result, the treated area becomes numb, and pain messages can no longer reach the brain. This effect is temporary once the medication wears off, nerve activity gradually returns to normal.
Clinically, this mechanism is essential for performing surgery or pain management safely without affecting the entire nervous system. Unlike general anesthetics, Naropin works locally, allowing patients to remain conscious and recover faster. Its formulation is also designed to minimize penetration into heart and brain tissues, reducing the likelihood of serious cardiovascular or central nervous system side effects compared to older anesthetics like bupivacaine.
Naropin side effects
Naropin is generally well tolerated when administered by trained medical professionals. However, as with any anesthetic, side effects can occur, most of which are mild and resolve as the drug wears off.
Common side effects may include:
- Nausea or vomiting
- Dizziness or lightheadedness
- Low blood pressure
- Temporary numbness or tingling beyond the target area
- Mild itching or back pain at the injection site
Serious but rare side effects may include:
- Irregular heartbeat or chest pain
- Difficulty breathing or swallowing
- Seizures or loss of consciousness (in cases of overdose or accidental injection into a blood vessel)
- Signs of allergic reaction such as rash, swelling, or trouble breathing
Because Naropin acts directly on the nervous system, proper dosing and careful monitoring are crucial. Anesthesiologists use specialized techniques to ensure the drug stays in the correct location and concentration.
Inform your doctor about severe liver disease, certain heart conditions, or amide-type anesthetic allergies before Naropin. Seek immediate medical help for confusion, tremors, or severe dizziness, as these may indicate anesthetic toxicity.
Naropin dosage
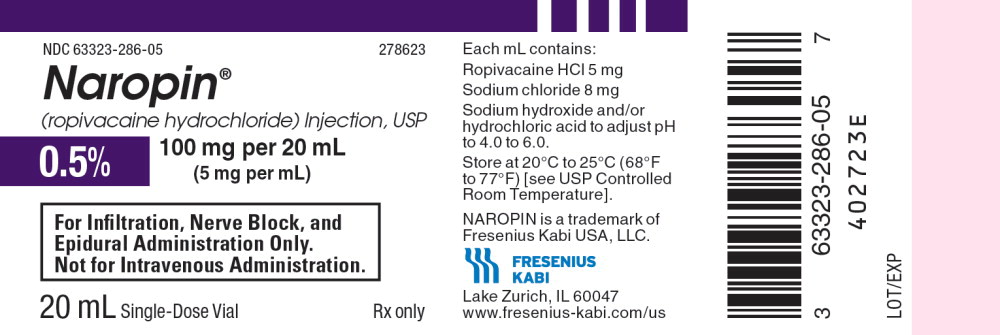
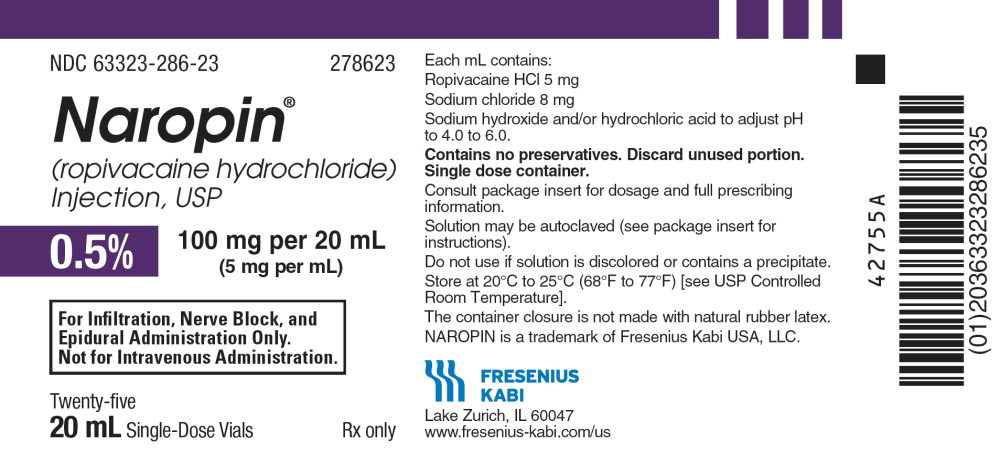
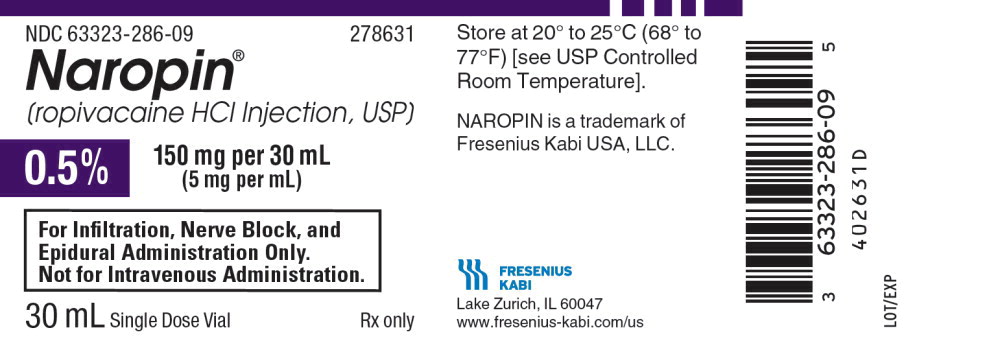
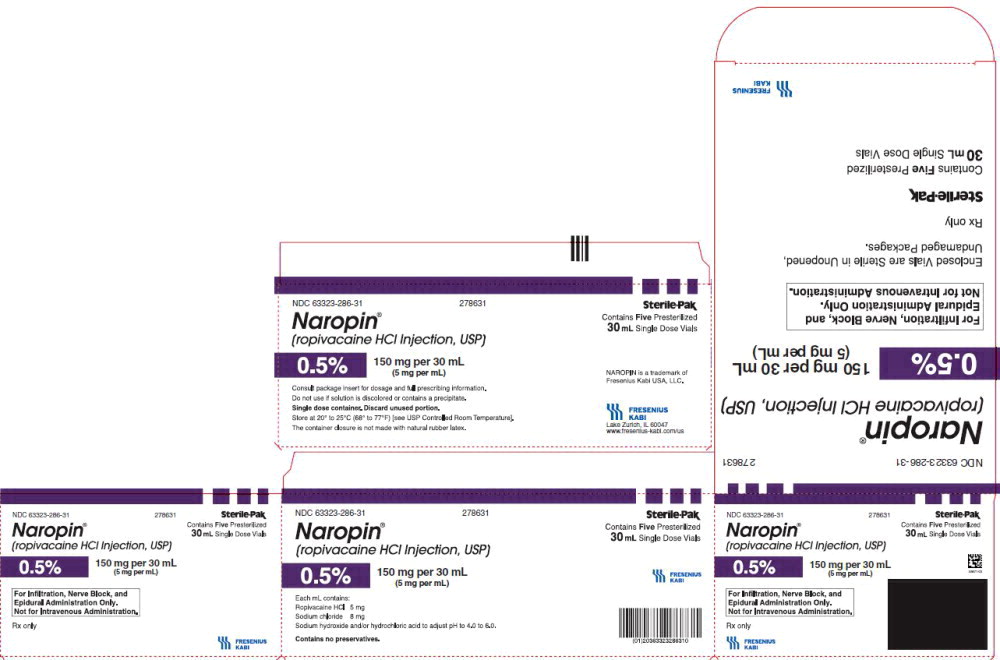
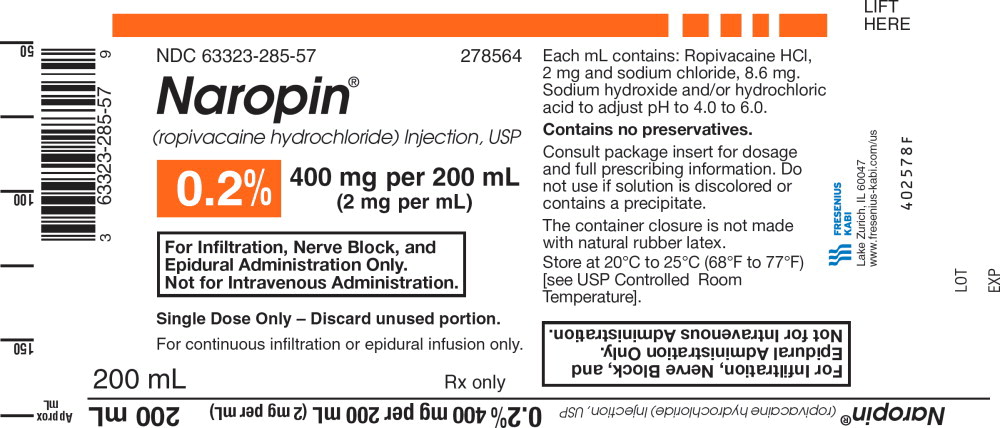
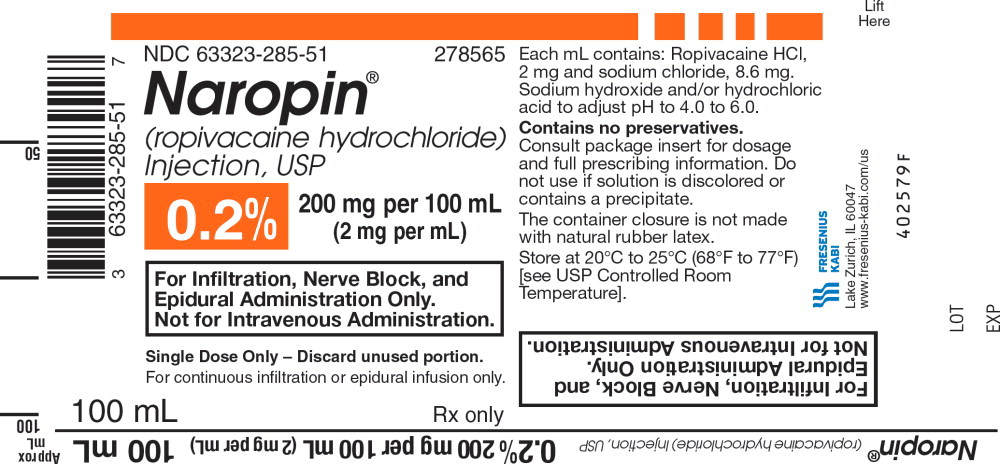
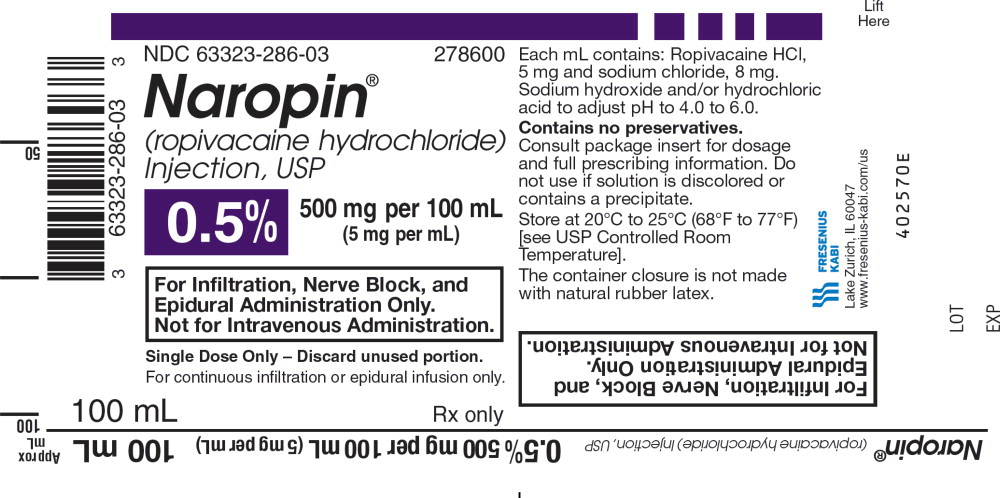
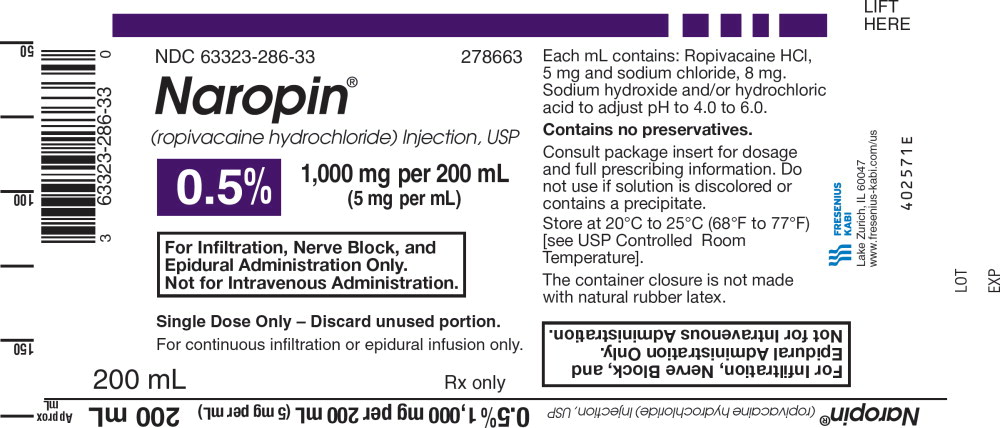
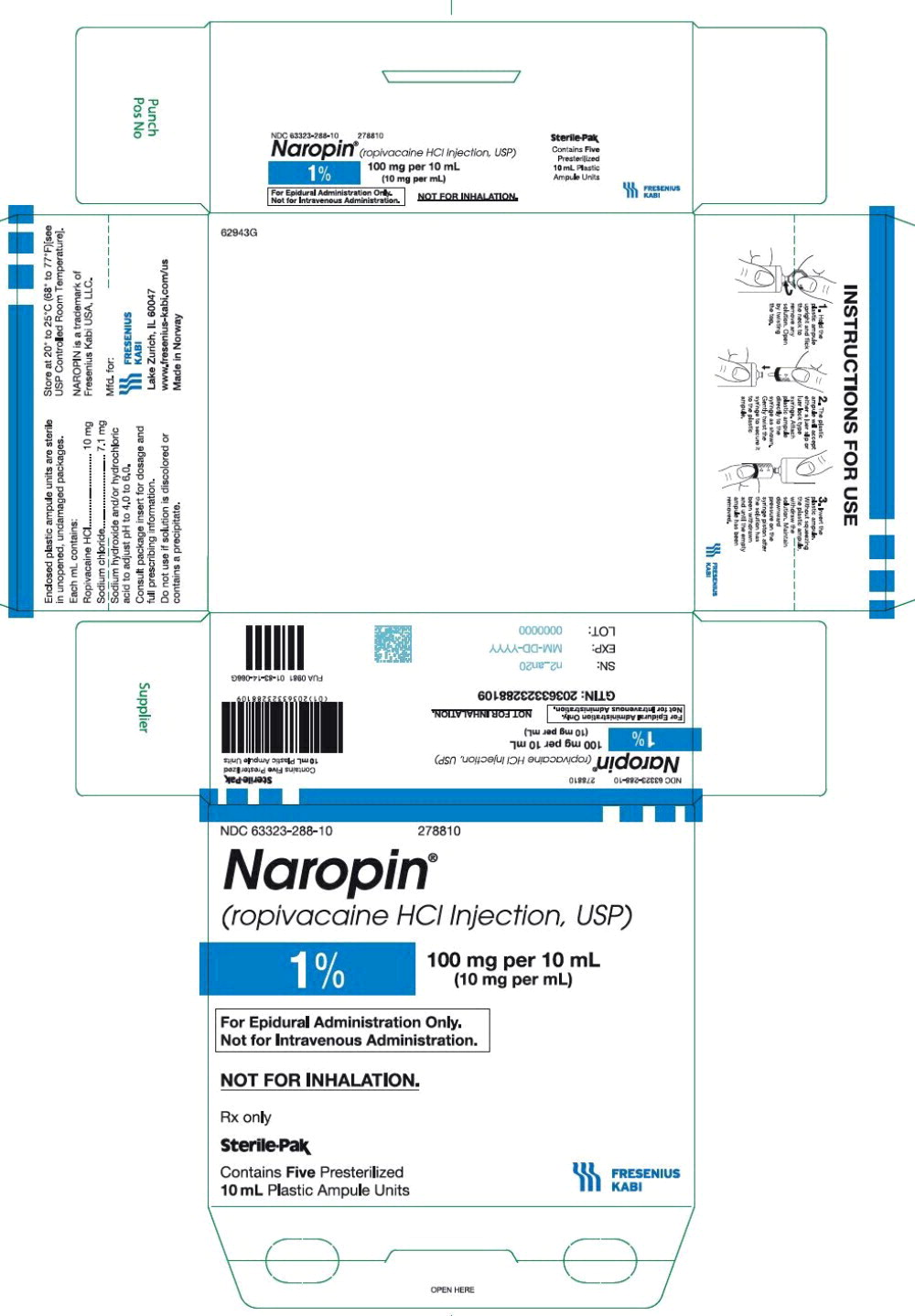
Naropin is an injectable or continuously infused anesthetic available in various strengths and volumes. Administered by trained professionals, common uses include epidural anesthesia, peripheral nerve blocks, local infiltration, and postoperative infusions. Dosing is individualized based on body size, surgery type, and desired anesthesia level.
Doctors monitor blood pressure, heart rate, oxygen, and overall patient response during and after administration. Special care is taken with older adults and patients with liver or cardiovascular disease due to slower drug metabolism, requiring dose adjustments for pain control and complication avoidance.
Does Naropin have a generic version?
Yes. Ropivacaine, the active ingredient in Naropin, is available in generic form and is FDA-approved in the United States and many other countries. Generic ropivacaine formulations are chemically and therapeutically equivalent to Naropin, offering the same level of effectiveness, safety, and duration of pain relief.
Generics lower treatment costs without sacrificing quality. Both Naropin and generic ropivacaine are common in medical settings, ensuring consistent patient care regardless of the version used.
Conclusion
Naropin (ropivacaine) is a trusted and effective local anesthetic widely used to prevent or control pain during and after surgical procedures. By blocking nerve signals in specific areas, it allows patients to undergo operations or childbirth comfortably and safely often while remaining awake and alert.
Naropin is a safe, effective, FDA-approved modern anesthetic used in regional anesthesia and pain management. Administered by professionals, it reduces surgical and recovery pain, providing comfort and confidence to patients.
References
- U.S. Food and Drug Administration (FDA). (2024). Naropin (ropivacaine) injection labeling information. Retrieved from https://www.accessdata.fda.gov
- Mayo Clinic. (2024). Ropivacaine (injection route) drug information. Retrieved from https://www.mayoclinic.org
- MedlinePlus. (2024). Ropivacaine injection: Uses, precautions, and side effects. National Library of Medicine. Retrieved from https://medlineplus.gov
- National Institutes of Health (NIH). (2024). Local anesthetics and regional pain management overview. Retrieved from https://www.nih.gov
Approved To Treat
Top Global Experts
There are no experts for this drug
Related Clinical Trials
There is no clinical trials being done for this treatment
Related Latest Advances
There is no latest advances for this treatment
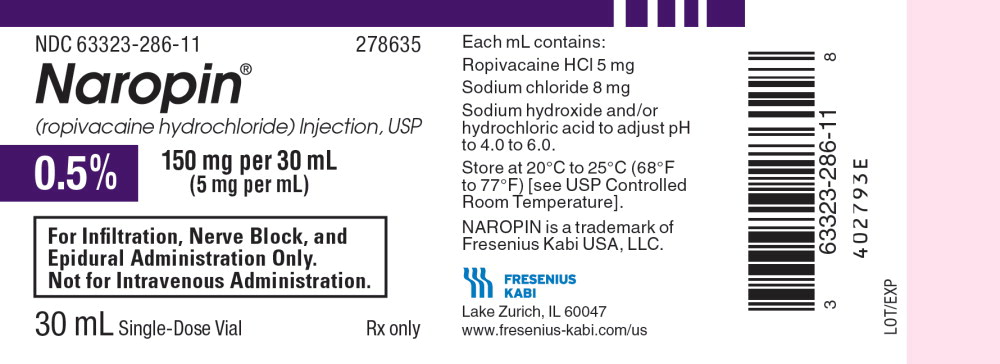
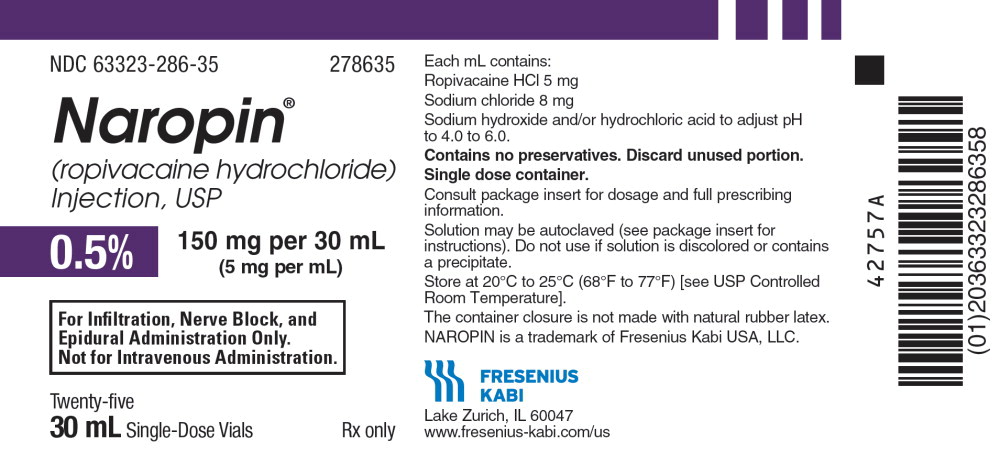
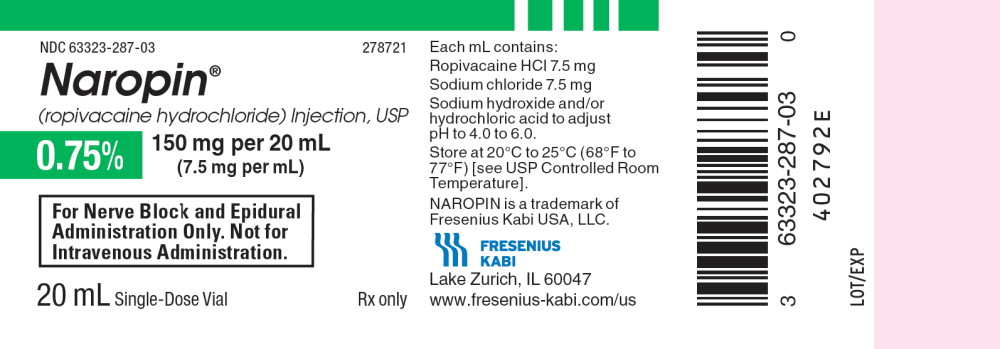
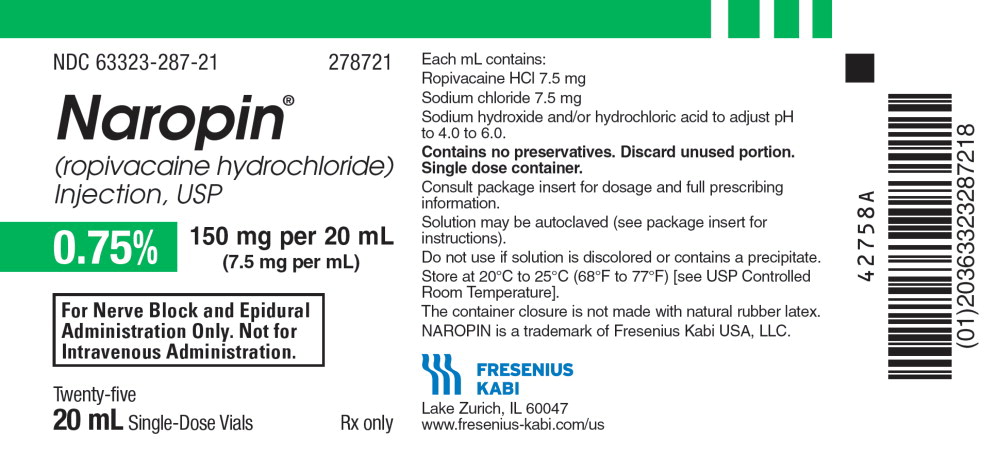
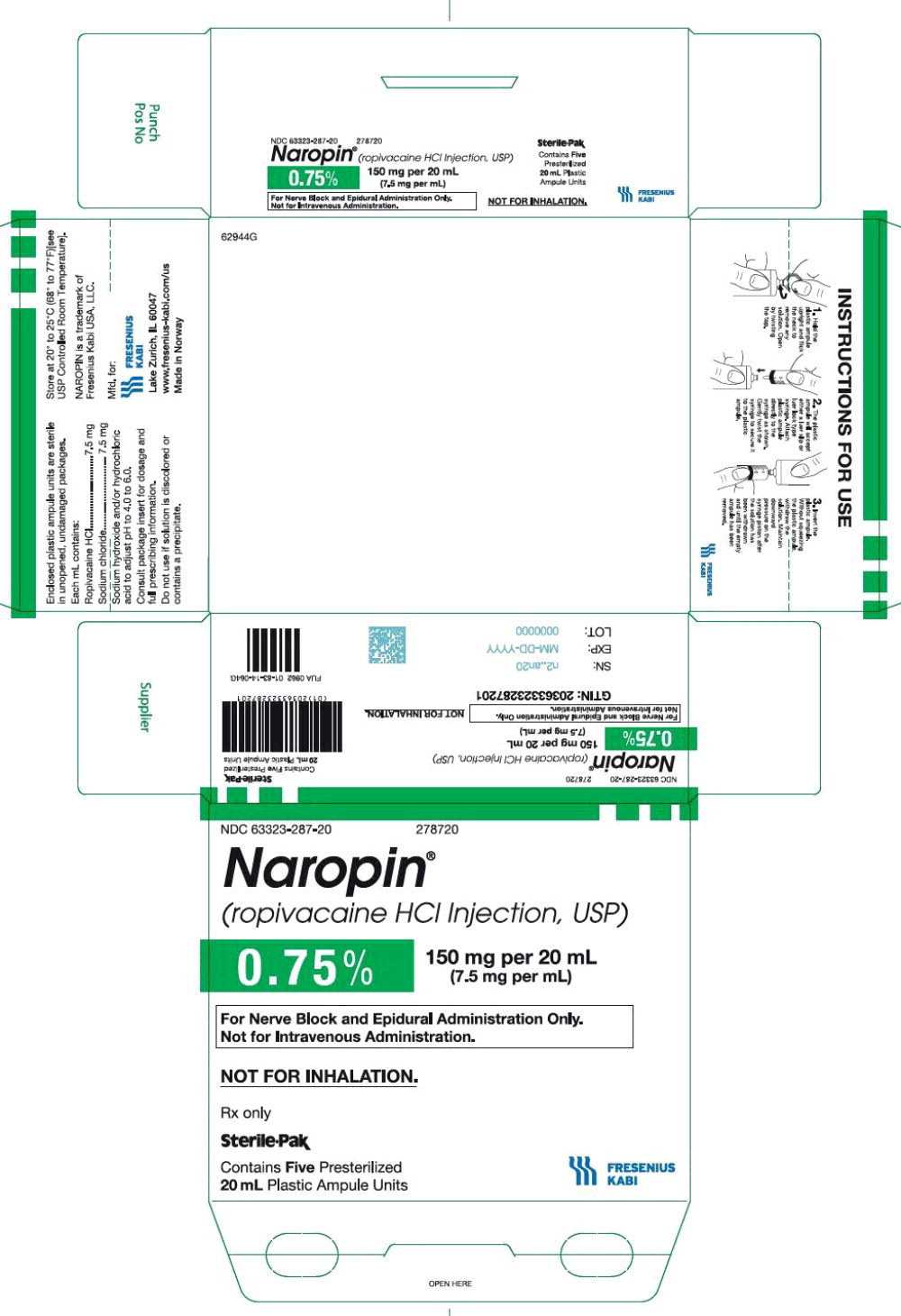
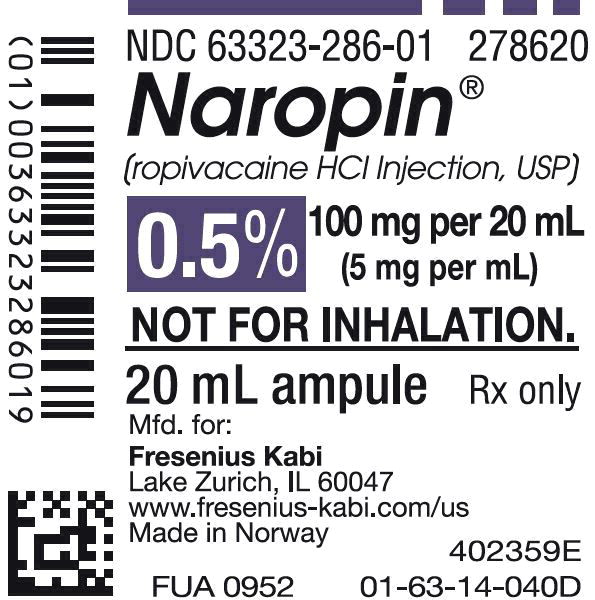
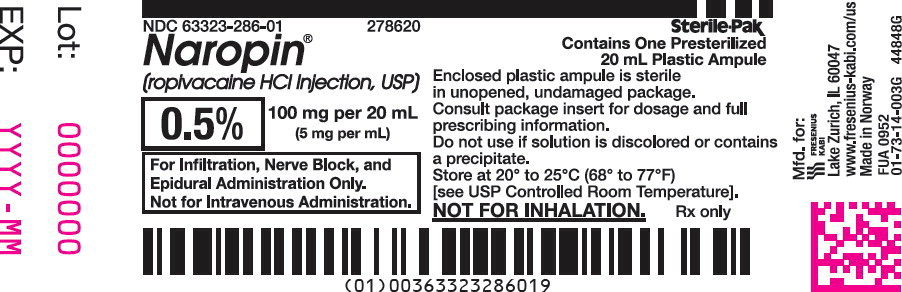
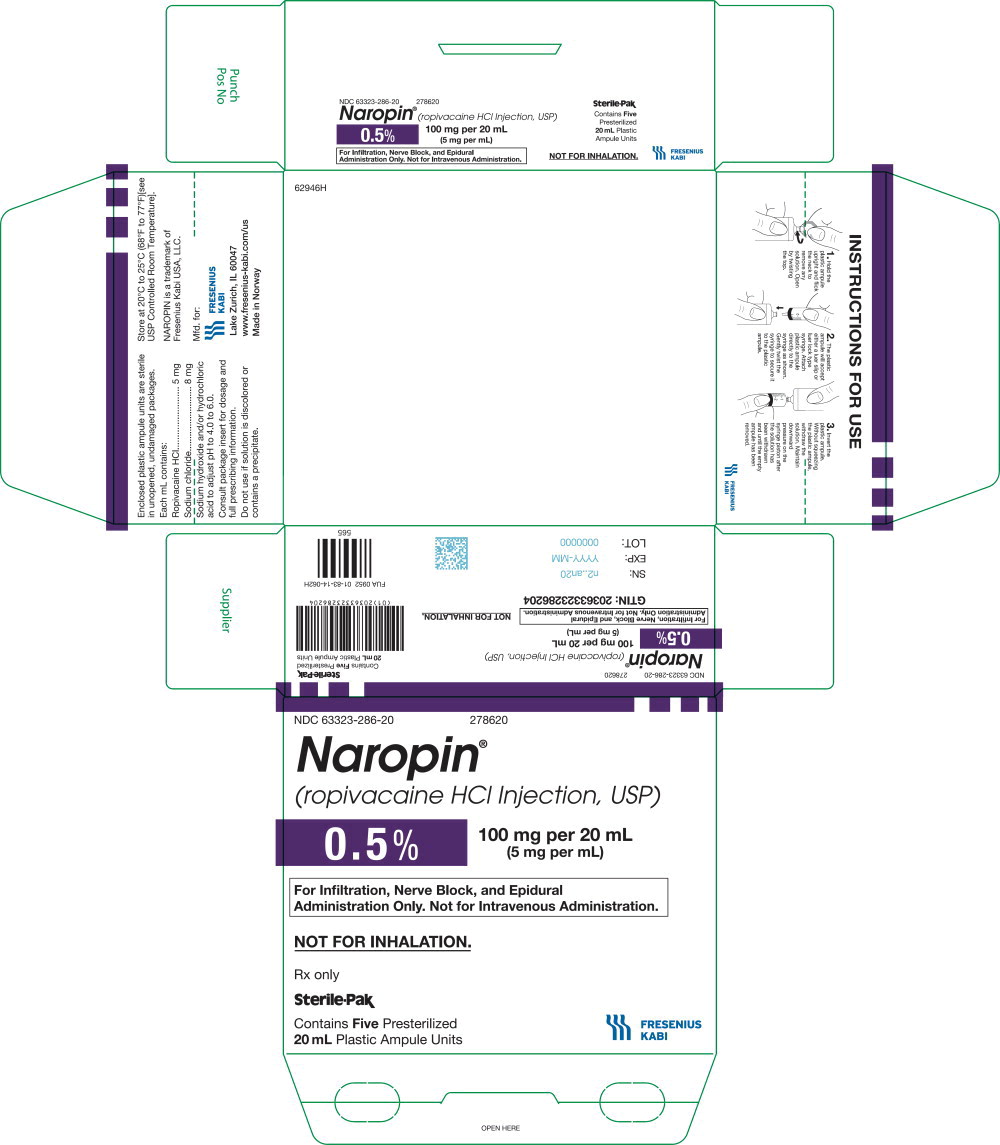
Brand Information
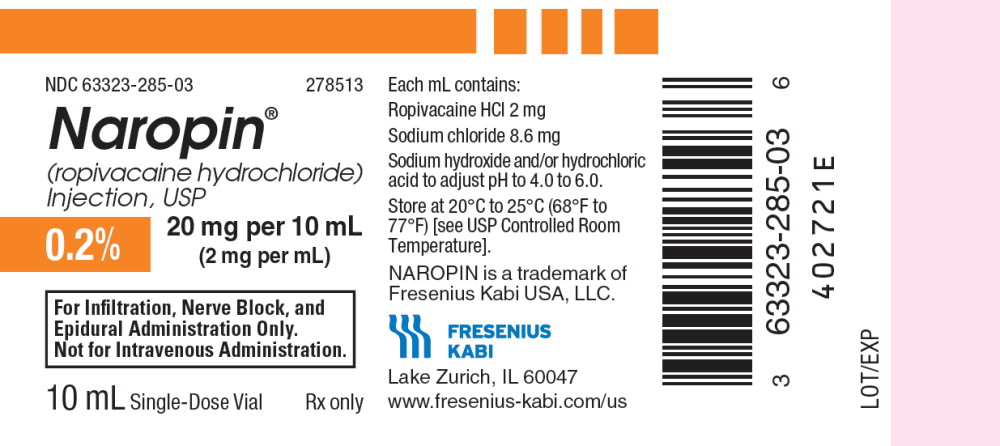
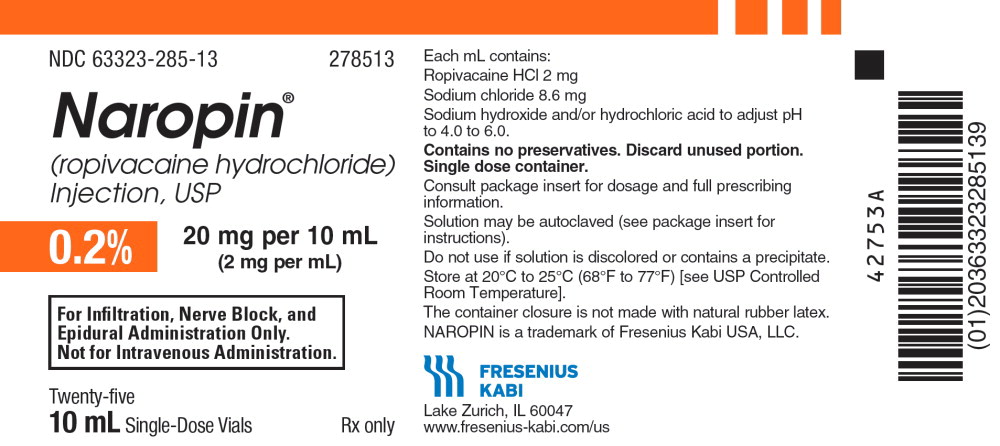
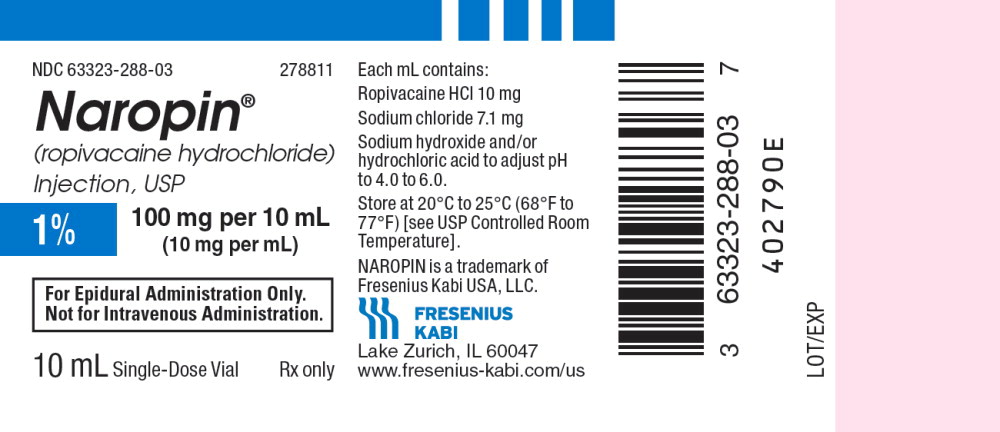
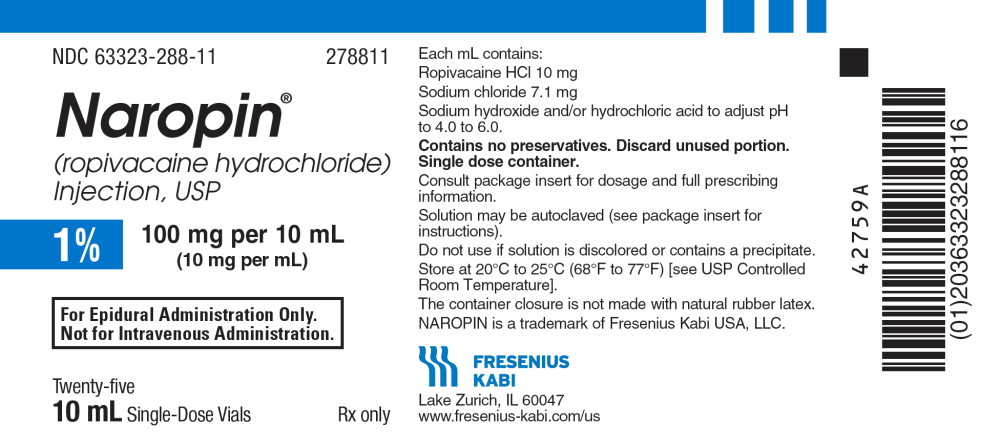
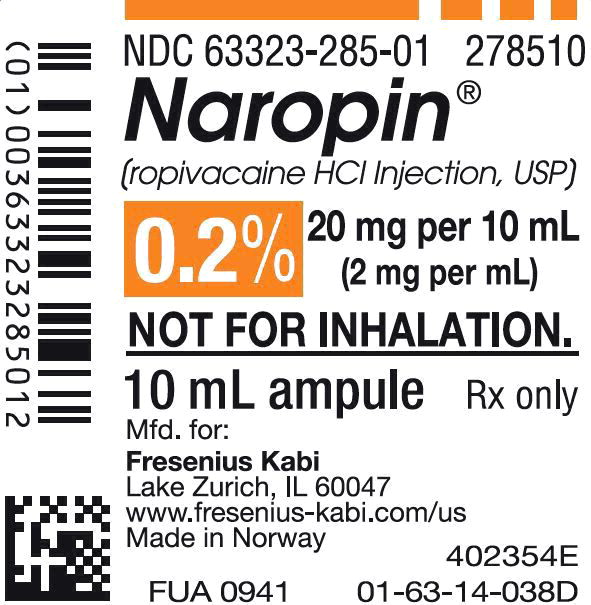
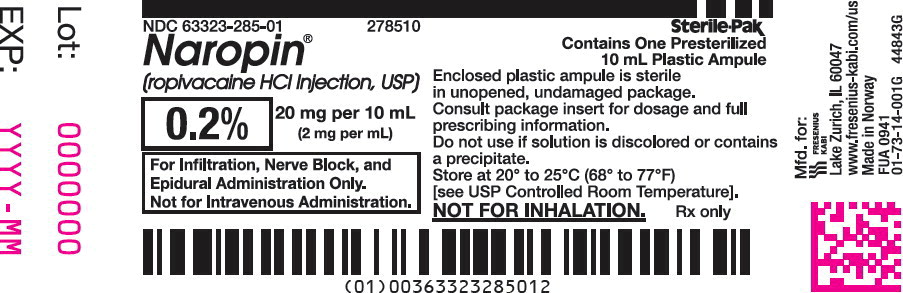
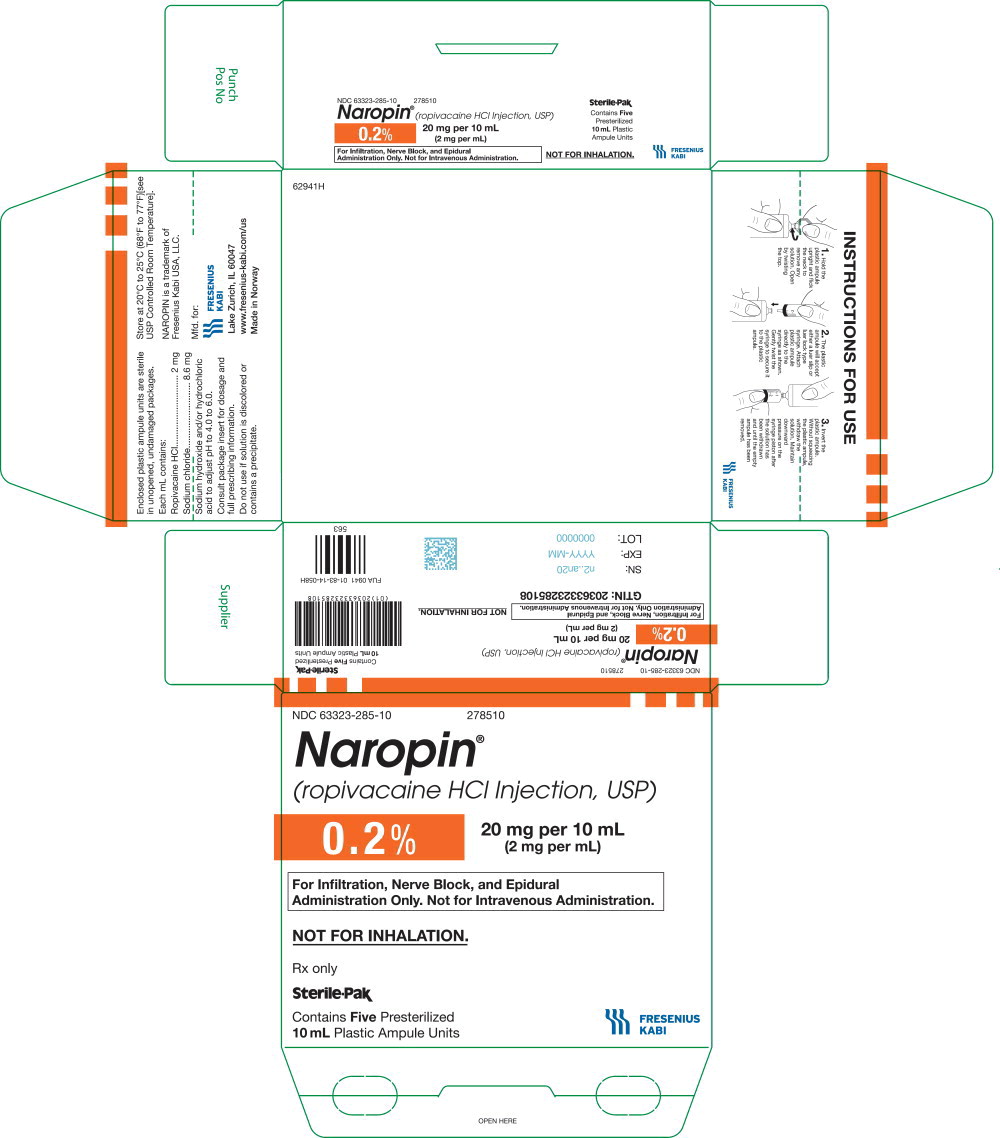
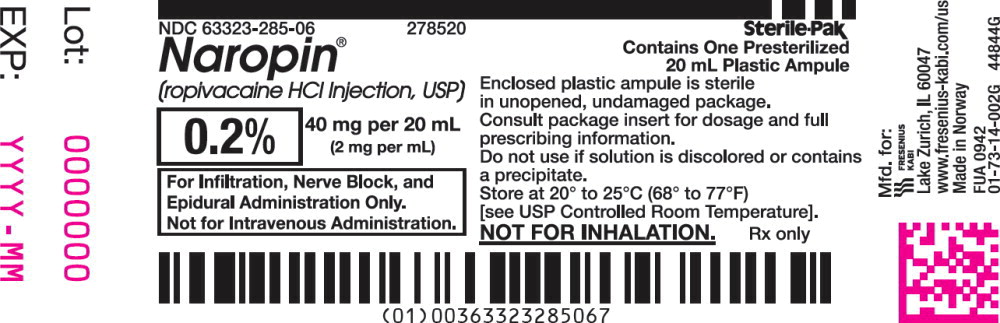
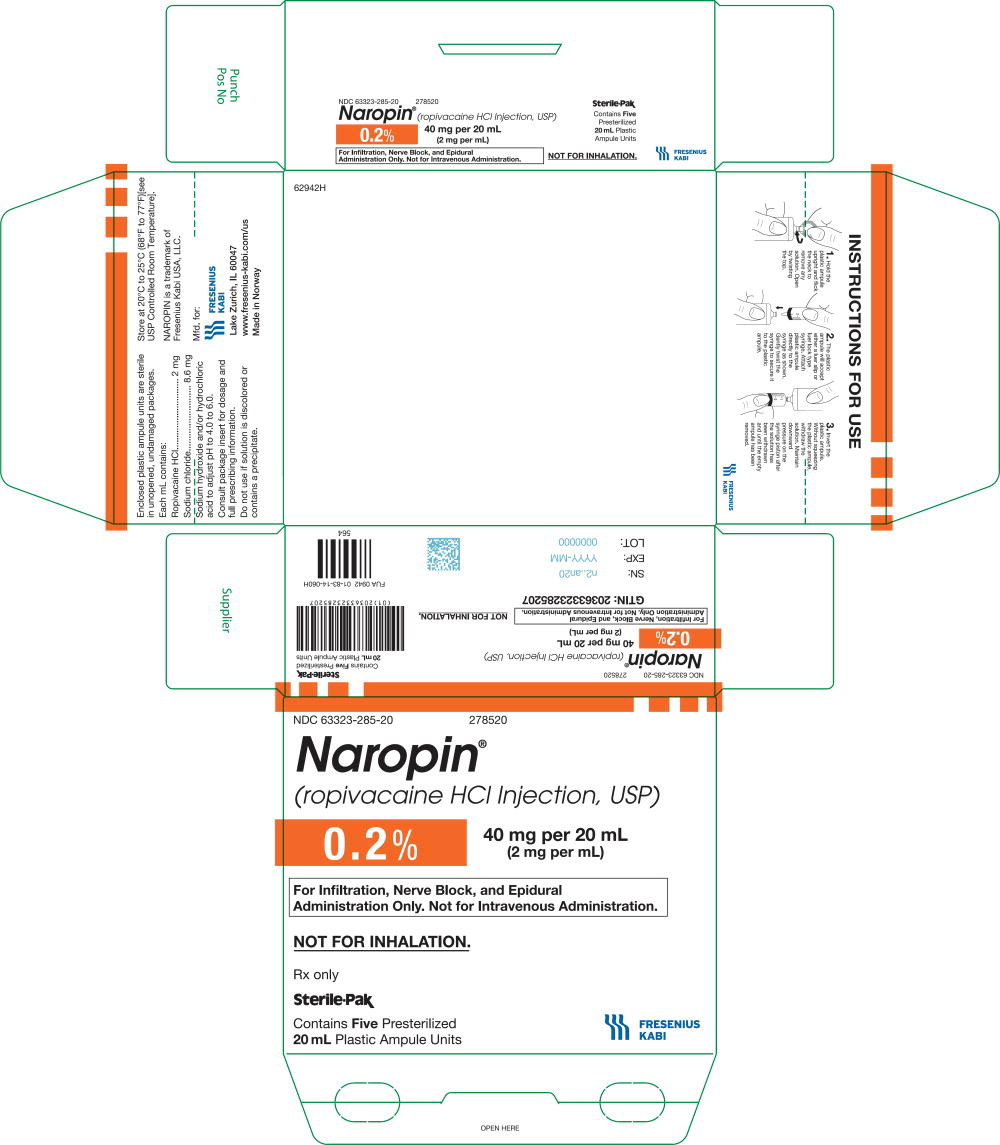
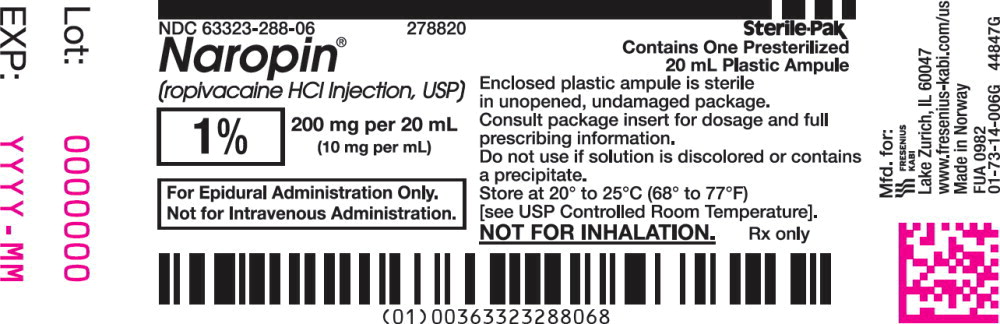
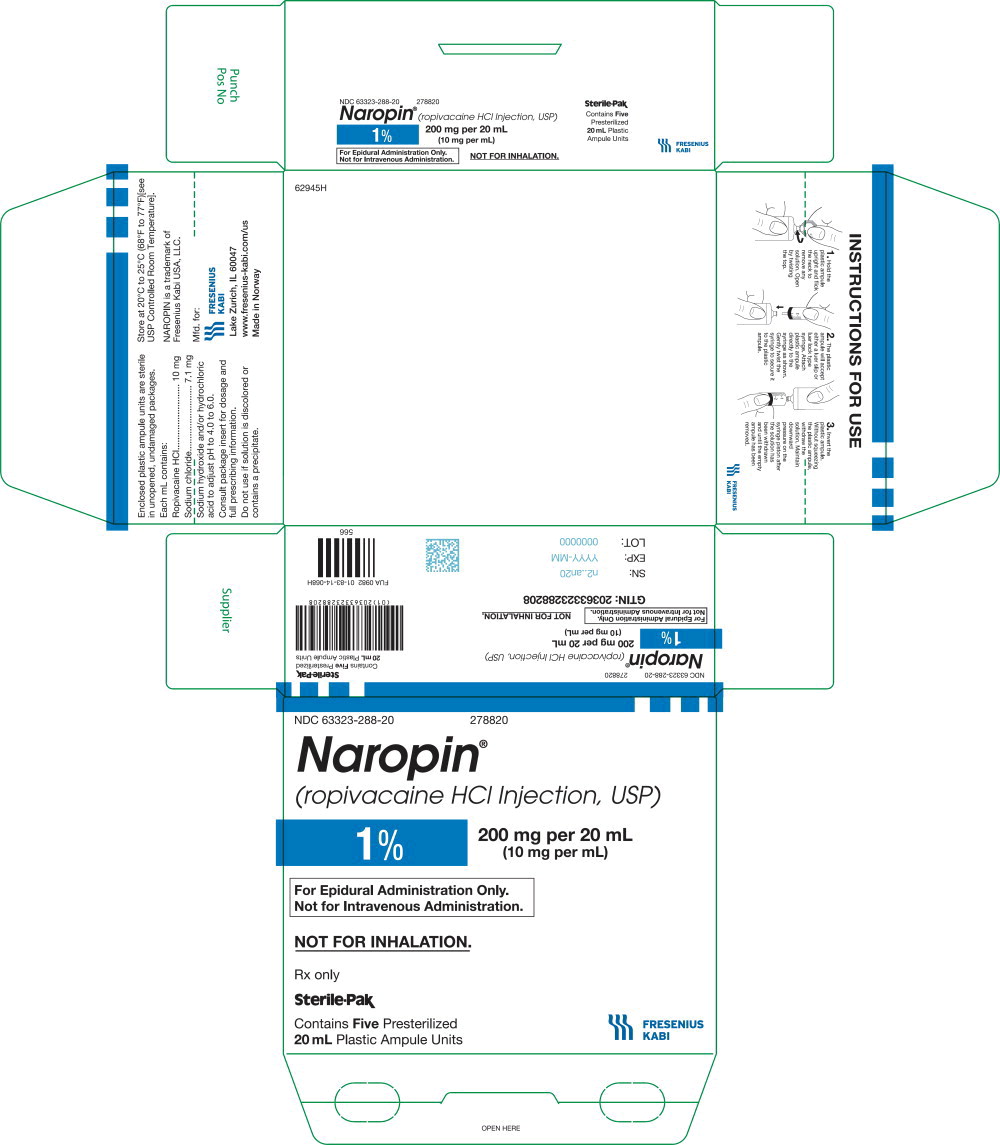
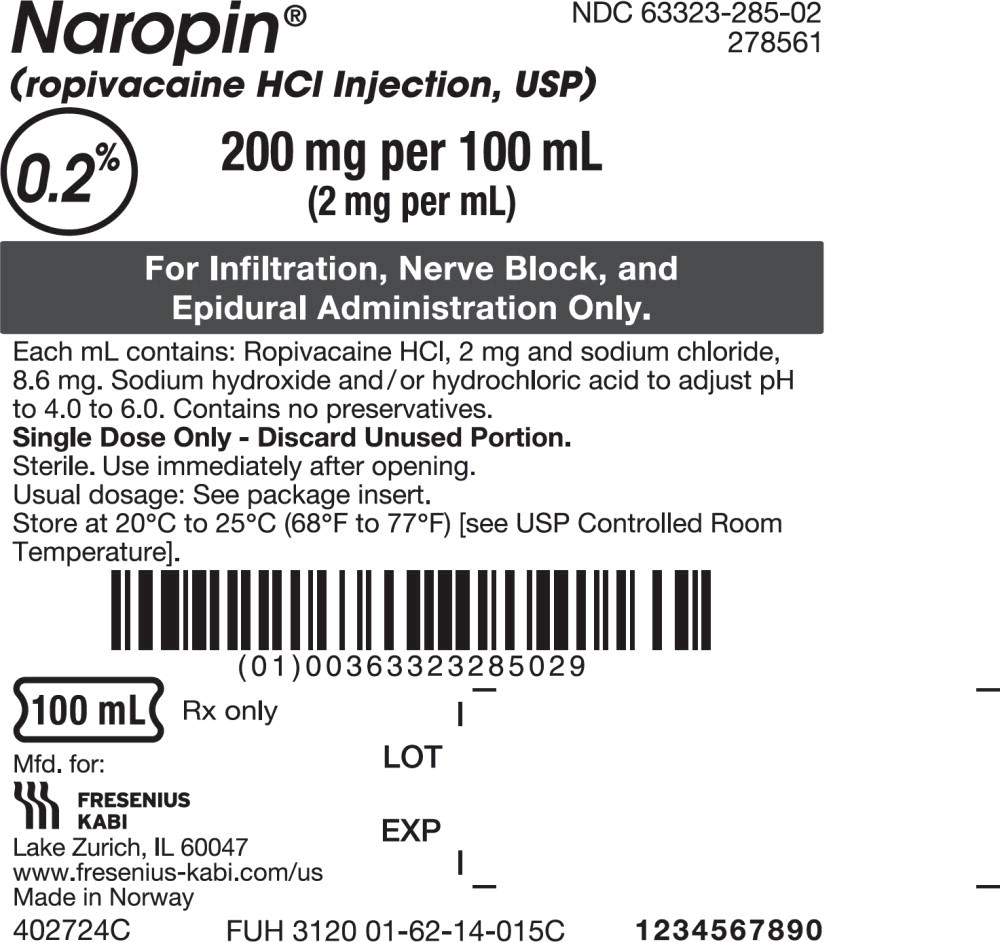
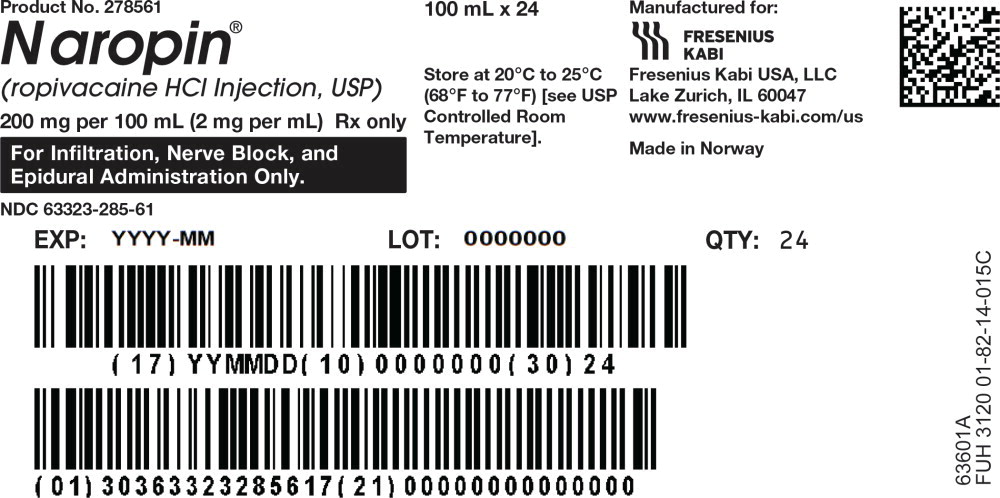
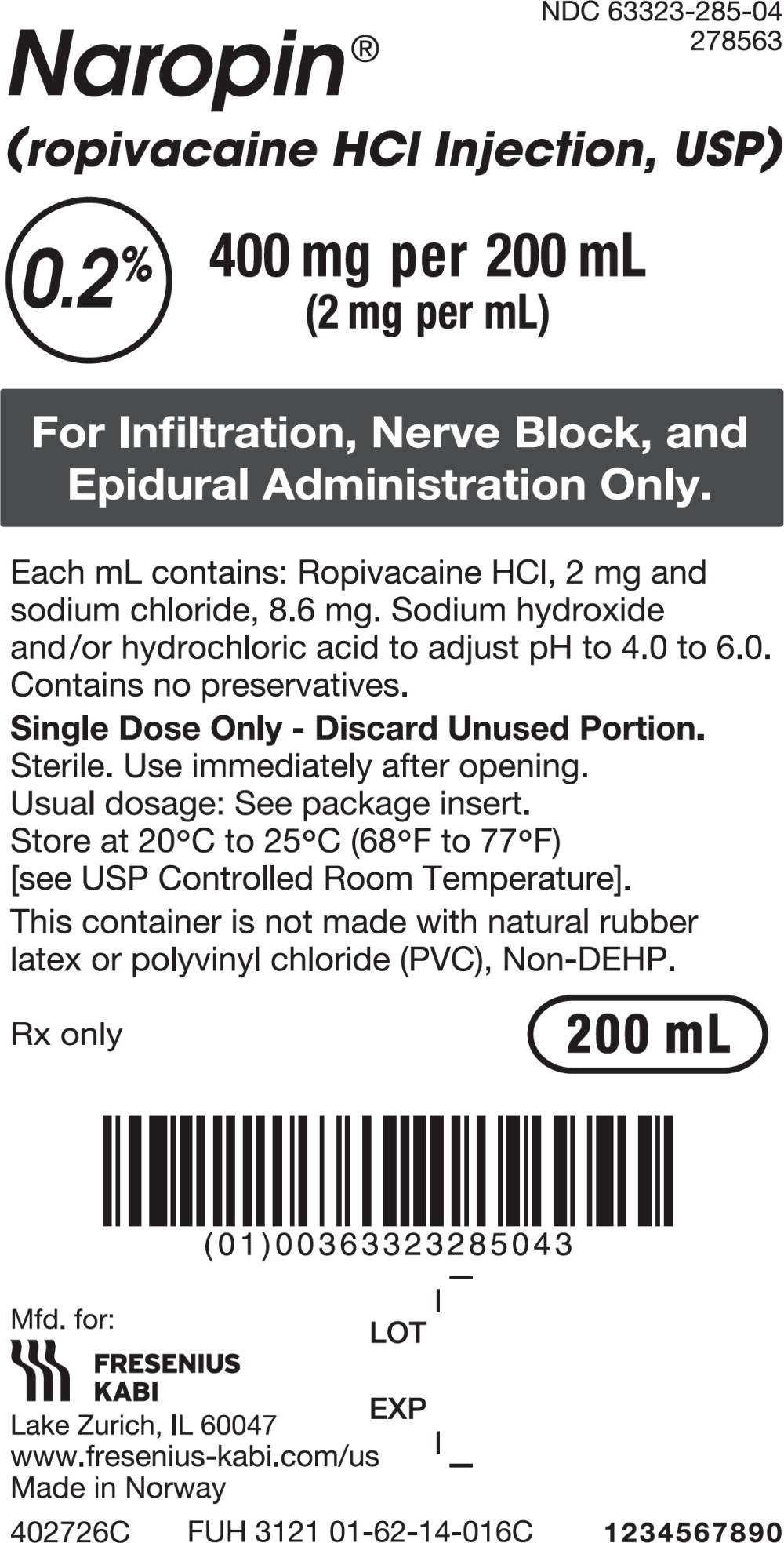
- 0.2%, 20 mg per 10 mL (2 mg/mL), in 10 mL single-dose vial
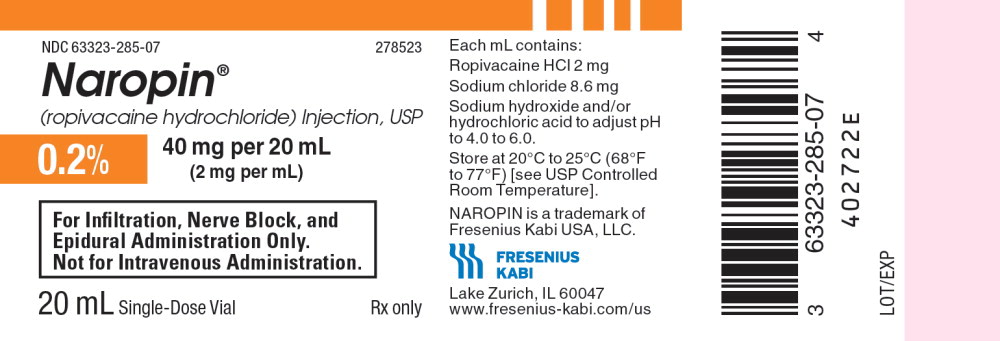
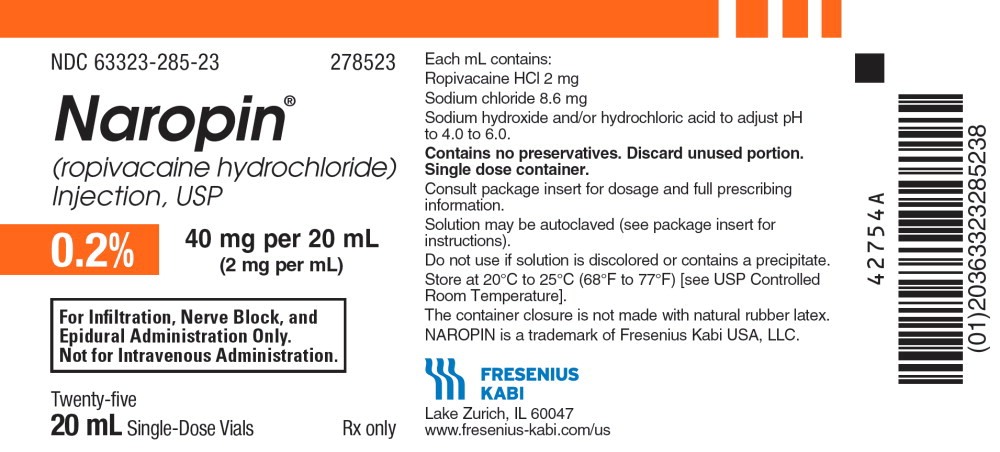
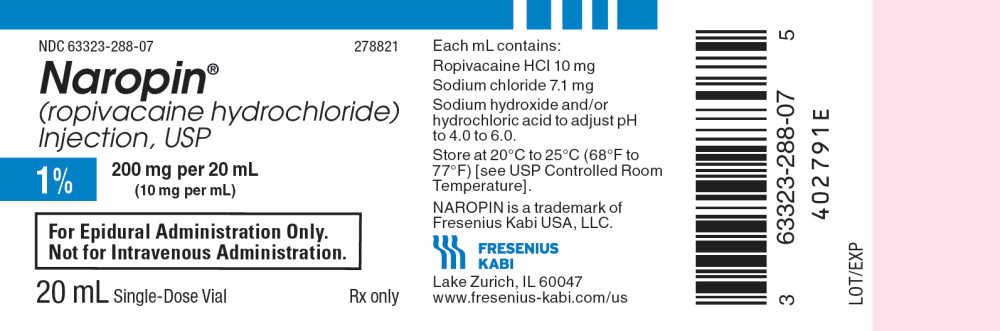
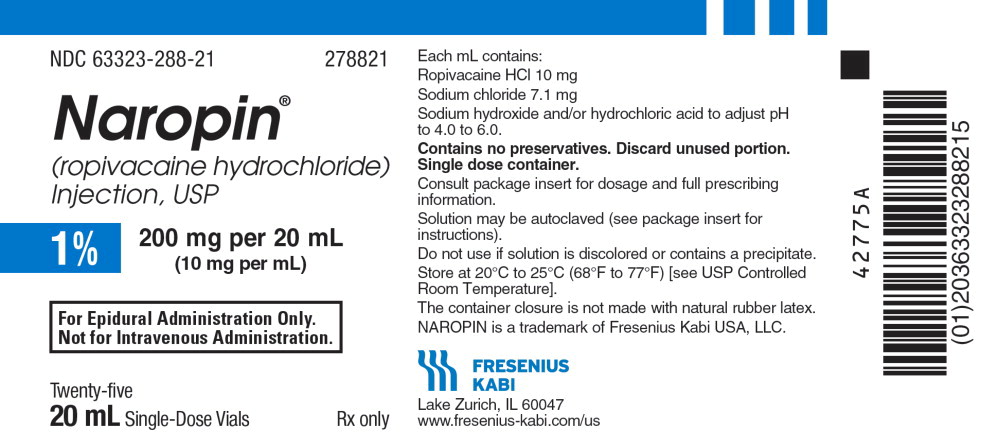
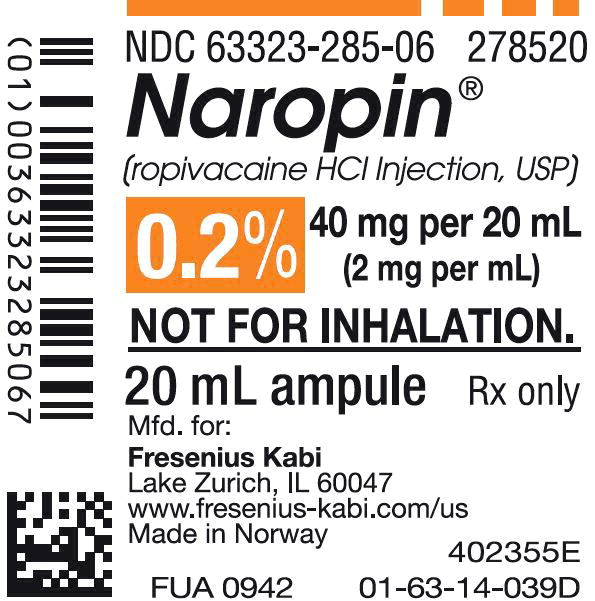
- 0.2%, 40 mg per 20 mL (2 mg/mL), in 20 mL single-dose vial
- 0.5%, 100 mg per 20 mL (5 mg/mL), 20 mL single-dose vial
- 0.5%, 150 mg per 30 mL (5 mg/mL), 30 mL single-dose vial
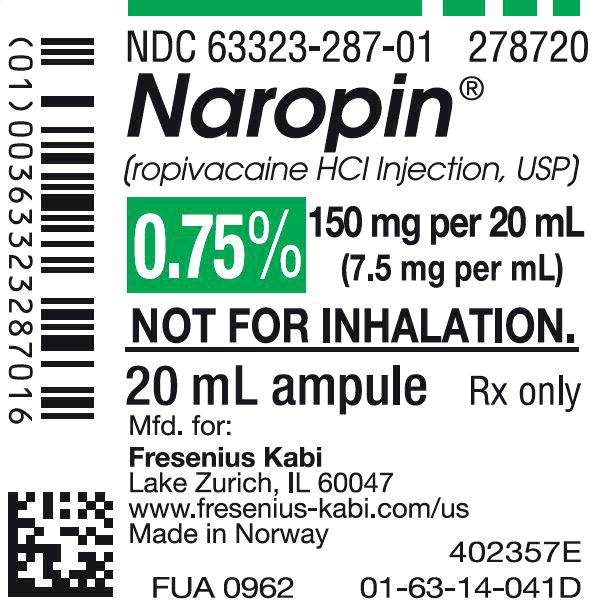
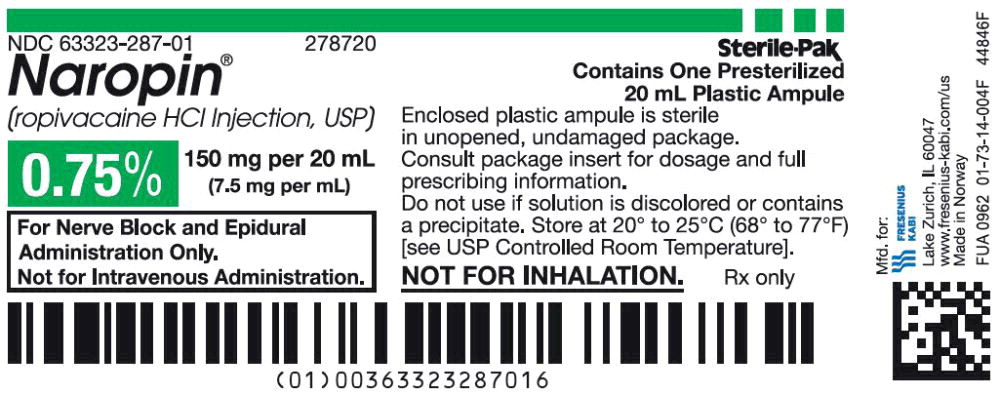
- 0.75%, 150 mg per 20 mL (7.5 mg/mL), 20 mL single-dose vial
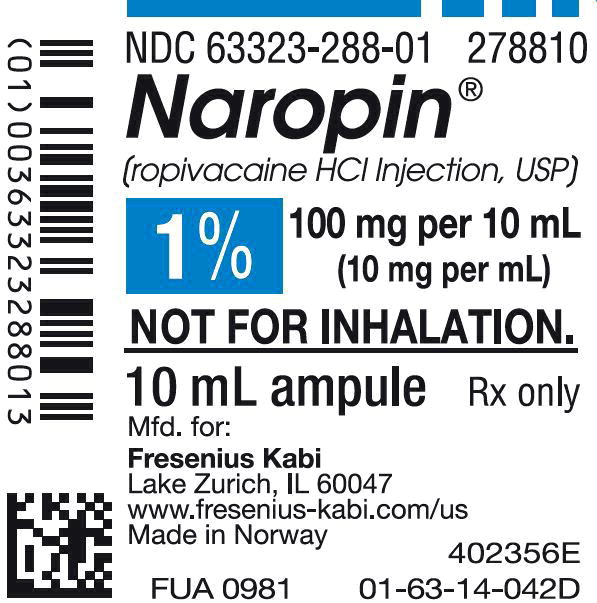
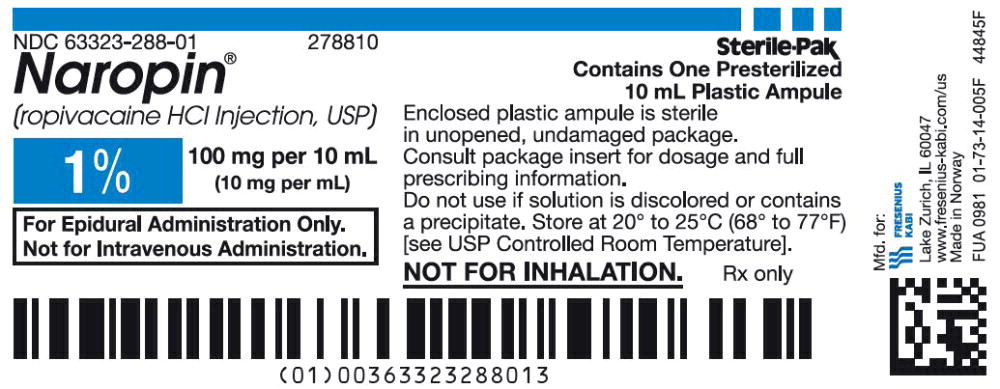
- 1%, 100 mg per 10 mL (10 mg/mL), 10 mL single-dose vial
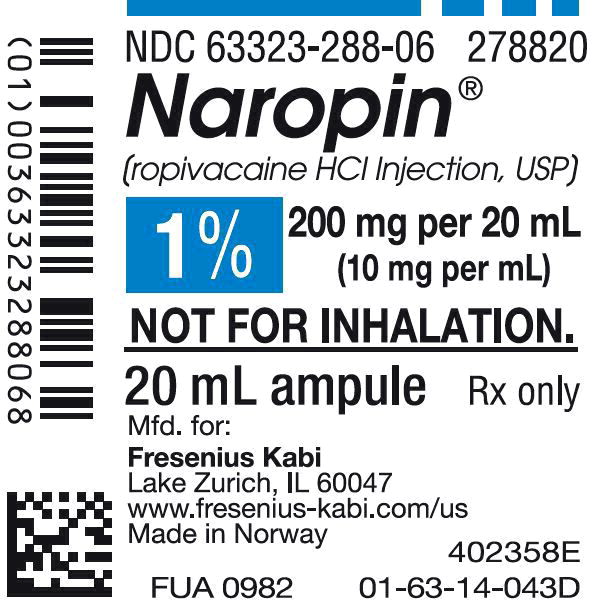
- 1%, 200 mg per 20 mL (10 mg/mL), 20 mL single-dose vial
- 0.2%, 200 mg per 100 mL (2 mg/mL), 100 mL single-dose infusion bottle
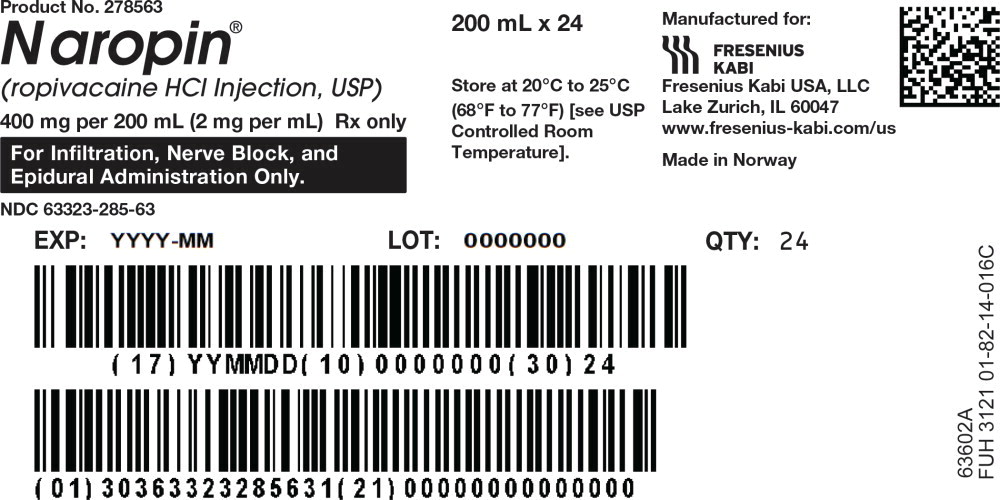
- 0.2%, 400 mg per 200 mL (2 mg/mL ), 200 mL single-dose infusion bottle
- 0.5%, 500 mg per 100 mL (5 mg/mL), 100 mL single-dose infusion bottle
- 0.5%, 1,000 mg per 200 mL (5 mg/mL ), 200 mL single-dose infusion bottle
- 0.2%, 20 mg per 10 mL (2 mg/mL), 10 mL single-dose polypropylene ampule
- 0.2%, 40 mg per 20 mL (2 mg/mL), 20 mL single-dose polypropylene ampule
- 0.5%, 100 mg per 20 mL (5 mg/mL), 20 mL single-dose polypropylene ampule
- 0.75%, 150 mg per 20 mL (7.5 mg/mL), 20 mL single-dose polypropylene ampule
- 1%, 100 mg per 10 mL (10 mg/mL), 10 mL single-dose polypropylene ampule
- 1%, 200 mg per 20 mL (10 mg/mL), 20 mL single-dose polypropylene ampule
- 0.2%, 200 mg per 100 mL (2 mg/mL), 100 mL single-dose, ready-to-use, polypropylene flexible bag
- 0.2%, 400 mg per 200 mL (2 mg/mL), 200 mL fill in 250 mL single-dose, ready-to-use, polypropylene flexible bag.