Tagrisso
What is Tagrisso (Osimertinib)?
Receiving a lung cancer diagnosis can be overwhelming, filled with uncertainty and questions about treatment options and survival. For many people with specific genetic forms of non-small cell lung cancer (NSCLC), Tagrisso (osimertinib) represents a major step forward in precision cancer therapy. This medication offers patients not just longer survival, but also a better quality of life, helping them breathe easier and live more fully during treatment.
Tagrisso is a targeted therapy used to treat certain types of lung cancer driven by mutations in the epidermal growth factor receptor (EGFR) gene. It belongs to a class of medications known as tyrosine kinase inhibitors (TKIs), which work by blocking abnormal signals that cause cancer cells to grow and spread. Approved by the U.S. Food and Drug Administration (FDA) in 2015, Tagrisso is now considered a first-line treatment for patients with EGFR-mutated NSCLC. It can also be used when the cancer has progressed after earlier EGFR-targeted treatments or when it has spread to the brain.
What does Tagrisso do?
Tagrisso is prescribed to treat non-small cell lung cancer (NSCLC) in adults whose tumors have specific EGFR gene mutations, such as exon 19 deletions or exon 21 (L858R) substitutions. These mutations cause cancer cells to grow uncontrollably, and Tagrisso is designed to block the signals driving this growth.
Doctors may prescribe Tagrisso in several settings:
- As a first-line therapy for newly diagnosed EGFR-mutated NSCLC.
- After previous EGFR therapy if the cancer develops a T790M resistance mutation.
- As adjuvant treatment after surgery to reduce the risk of cancer returning.
Clinical studies have shown that Tagrisso can extend overall survival and delay disease progression more effectively than earlier EGFR inhibitors. In the pivotal FLAURA trial, patients taking Tagrisso lived a median of nearly 39 months, compared with about 31 months for those taking older EGFR-targeted drugs (FDA, 2024).
Many patients also experience improved control of cancer that has spread to the brain or spinal cord, since Tagrisso can cross the blood-brain barrier, something earlier drugs in its class often cannot do.
How does Tagrisso work?
Tagrisso (osimertinib) targets and blocks abnormal EGFR proteins found on the surface of cancer cells. These proteins send continuous “grow and divide” signals that cause uncontrolled tumor growth.
By binding to the mutated EGFR receptor, Tagrisso stops the cancer’s internal signaling pathway, slowing or stopping cell growth. It also works against tumors with the T790M mutation, a common cause of resistance to older EGFR inhibitors such as erlotinib or gefitinib.
In simpler terms, Tagrisso helps turn off the “growth switch” in cancer cells while sparing most normal cells. This selective action often results in fewer severe side effects than traditional chemotherapy, allowing many patients to continue normal daily activities during treatment.
Clinically, this mechanism is vital because it helps control tumor growth, delay progression, and improve survival outcomes for patients with specific genetic profiles, making Tagrisso a cornerstone in personalized cancer medicine.
Tagrisso side effects
While Tagrisso is generally well-tolerated, it can cause side effects. Most are mild to moderate, but some require close monitoring or medical attention.
Common side effects include:
- Diarrhea
- Rash or dry skin
- Fatigue
- Nail changes or mild hair thinning
- Cough or mild shortness of breath
These effects are usually manageable and tend to improve over time with supportive care.
Serious side effects (less common) include:
- Heart rhythm problems (QT prolongation): This can cause irregular heartbeat or fainting. Doctors often monitor heart function during treatment.
- Interstitial lung disease (ILD): A rare but potentially serious inflammation of lung tissue. Patients should contact their doctor if they develop sudden worsening cough, fever, or breathing difficulty.
- Eye or vision changes: Blurred vision, eye pain, or swelling should be reported immediately.
- Low blood cell counts: Routine blood tests help ensure healthy levels of red and white cells and platelets.
Patients with heart disease, lung conditions, or electrolyte imbalances should inform their doctor before starting Tagrisso.
Emergency medical attention is required for symptoms like chest pain, severe shortness of breath, swelling, or severe skin reactions. Despite these potential risks, most patients tolerate the medication well, especially compared to conventional chemotherapy.
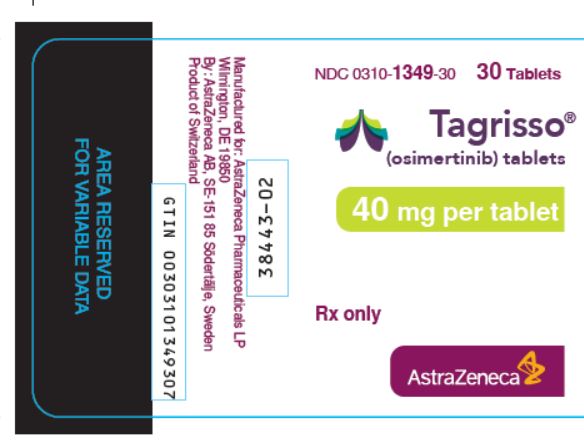
Tagrisso dosage
Tagrisso is an oral tablet taken once daily, with or without food, offering convenient at-home treatment. Consistency is vital; take it at the same time daily to maintain stable drug levels. Do not crush or chew unless directed by a healthcare professional.
Doctors regularly monitor patients using blood tests (liver/kidney function), ECGs (heart rhythm), and scans (tumor response). Severe side effects may lead to temporary dose adjustments. Caution is needed for older adults or those with existing heart/lung conditions due to potential medication processing influences.
Does Tagrisso have a generic version?
As of 2025, Tagrisso (osimertinib) does not have a generic version available in the United States or most other countries. It is currently manufactured exclusively by AstraZeneca. However, international versions may exist in other markets.
Tagrisso’s patent is active, so generics aren’t expected soon. International access programs and patient assistance may offer cost relief. Approved generics will be FDA-certified as equivalent. Discuss financial support and insurance with your oncologist or pharmacist.
Conclusion
Tagrisso (osimertinib) has transformed the outlook for many people living with EGFR-mutated non-small cell lung cancer. By precisely targeting the molecular drivers of tumor growth, it offers an effective, well-tolerated, and convenient treatment that can significantly extend survival and maintain quality of life.
Under medical supervision, Tagrisso is a safe and effective option for most eligible patients. With consistent use and open communication, it offers hope for longer, easier breathing and renewed strength.
References
- U.S. Food and Drug Administration (FDA). (2024). Tagrisso (osimertinib) prescribing information. Retrieved from https://www.accessdata.fda.gov
- Mayo Clinic. (2024). Osimertinib (oral route) description and precautions. Retrieved from https://www.mayoclinic.org
- MedlinePlus. (2024). Osimertinib: Uses, side effects, and warnings. National Library of Medicine. Retrieved from https://medlineplus.gov
- National Institutes of Health (NIH). (2024). Targeted therapy for non-small cell lung cancer (NSCLC). Retrieved from https://www.nih.gov
Approved To Treat
Top Global Experts
Related Clinical Trials
Summary: This phase II trial studies how well osimertinib works in treating patients with non-small cell lung cancer with EGFR exon 20 insertion mutation that is stage IIIB-IV or has come back after a period of improvement (recurrent). Osimertinib may stop the growth of tumor cells by blocking some of the enzymes needed for cell growth.
Summary: This phase III trial compares the effect of adding stereotactic body radiation therapy (SBRT) to the usual treatment (conventional image guided radiation therapy \[IGRT\] and chemotherapy followed by immunotherapy with durvalumab or targeted therapy with osimertinib) versus the usual treatment alone in treating patients with non-small cell lung cancer that has spread to nearby tissue or lymph node...
Summary: The purpose of this study is to evaluate the safety, tolerability, drug levels, and preliminary efficacy of BMS-986507 combinations in adult participants with advanced solid tumors.
Related Latest Advances
Brand Information
- Interstitial Lung Disease/Pneumonitis
- QTc Interval Prolongation
- Cardiomyopathy
- Keratitis
- Erythema multiforme, Stevens-Johnson syndrome, and Toxic epidermal necrolysis
- Cutaneous Vasculitis
- Aplastic Anemia
- Skin and subcutaneous tissue: Erythema multiforme major (EMM), Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), cutaneous vasculitis, erythema dyschromicum perstans
- Blood and lymphatic system disorders: Aplastic anemia

- Inform patients of the risks of severe or fatal ILD, including pneumonitis. Advise patients to contact their healthcare provider immediately to report new or worsening respiratory symptoms
- Inform patients of symptoms that may be indicative of significant QTc prolongation including dizziness, lightheadedness, and syncope. Advise patients to report these symptoms and to inform their physician about the use of any heart or blood pressure medications
- Inform patients that TAGRISSO can cause cardiomyopathy. Advise patients to immediately report any signs or symptoms of heart failure to their healthcare provider
- Advise patients to contact their healthcare provider immediately if they develop eye symptoms (eye inflammation, lacrimation, light sensitivity, eye pain, red eye or changes in vision)
- Inform patients of signs and symptoms that may be indicative of EMM, SJS, or TEN. Advise patients to contact their healthcare provider immediately if they develop target lesions or severe blistering or peeling of skin
- Inform patients of signs and symptoms that may be indicative of cutaneous vasculitis. Advise patients to contact their healthcare provider immediately if they develop multiple, non-blanching red papules on their forearms, lower legs, or buttocks or large hives on their trunk that do not go away within 24 hours and develop a bruised appearance
- Inform patients of signs and symptoms of aplastic anemia including but not limited to new or persistent fevers, bruising, bleeding, pallor, infection, tiredness or weakness. Advise patients to contact their healthcare provider immediately if signs and symptoms suggestive of aplastic anemia develop
- Advise pregnant women and females of reproductive potential of the potential risk to a fetus. Advise females to inform their healthcare provider if they become pregnant or if pregnancy is suspected, while taking TAGRISSO
- Advise females of reproductive potential to use effective contraception during treatment with TAGRISSO and for 6 weeks after the last dose
- Advise males to use effective contraception during treatment and for 4 months after the last dose of TAGRISSO
- Advise women not to breastfeed during treatment with TAGRISSO and for 2 weeks after the last dose
Rx only

Rx only

Rx only
Rx only

