MediFind found 112 doctor with experience in Immune Thrombocytopenic Purpura (ITP) near Baltimore, MD. Of these, 55 are Experienced and 6 are Advanced.
Skip Viragh Outpatient Cancer Center
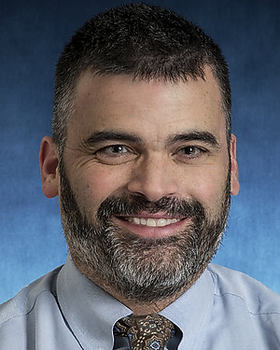
William Houck is an Oncologist in Baltimore, Maryland. Dr. Houck is rated as an Advanced provider by MediFind in the treatment of Immune Thrombocytopenic Purpura (ITP). His top areas of expertise are Paget Disease of the Breast, Lung Cancer, Chronic B-Cell Leukemia (CBCL), and Chronic Lymphocytic Leukemia (CLL).
The Johns Hopkins Hospital
Dr. Rakhi P. Naik is the Associate Director for the Division of Hematology at Johns Hopkins University. She also serves as Director of the Fellowship Hematology Track and Director of Organ Systems Foundation of Medicine (OSFM), the largest pre-clerkship course in the medical school. She holds an undergraduate degree in Biomedical & Electrical Engineering from Duke University, an M.D. with. Dr. Naik is rated as an Advanced provider by MediFind in the treatment of Immune Thrombocytopenic Purpura (ITP). Her top areas of expertise are Sickle Cell Disease, Congenital Hemolytic Anemia, Hemolytic Anemia, and Hemoglobinopathy.
Sidney Kimmel Comprehensive Cancer Center
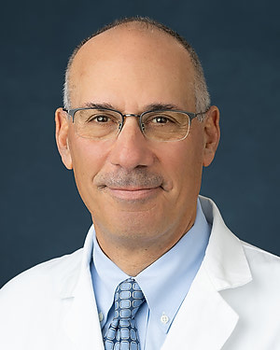
Dr. Robert Brodsky is a professor of medicine at the Johns Hopkins University School of Medicine. His area of clinical expertise is classical hematology and haploidentical bone marrow transplant for sickle cell disease and aplastic anemia. Dr. Brodsky serves as the director of the Division of Hematology and the T32 Training Program. He is the Johns Hopkins Family Professor of Medicine and Oncology. He received his M.D. from Hahnemann University. He completed his residency at the Vanderbilt University School of Medicine. He performed a fellowship in hematology at the National Institutes of Health and a fellowship in oncology at Johns Hopkins. He joined the Johns Hopkins faculty in 1997. From 2017 to 2022 he served as Associate Editor to The Journal of Clinical Investigation (JCI) and Secretary to American Society of Hematology (ASH). He serves as President of The American Society of Hematology (ASH) in 2023. Dr. Brodsky is rated as an Experienced provider by MediFind in the treatment of Immune Thrombocytopenic Purpura (ITP). His top areas of expertise are Paroxysmal Nocturnal Hemoglobinuria (PNH), Paroxysmal Cold Hemoglobinuria, Anemia, Bone Marrow Transplant, and Splenectomy.
Sidney Kimmel Comprehensive Cancer Center
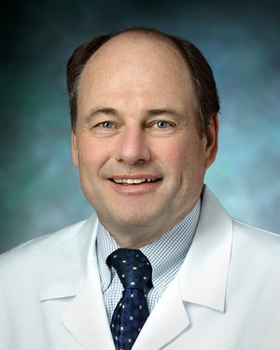
Dr. Lode J. Swinnen is a cancer specialist in Baltimore caring for patients with lymphoma. Dr. Swinnen received his M.B.Ch.B. degree from the University of Cape Town Medical School. He completed his residency at Presence Saint Joseph Hospital and performed a fellowship in hematology-oncology at Loyola University Stritch School of Medicine. Dr. Swinnen joined the Johns Hopkins faculty in 2002. His research interests include lymphomas and immunodeficiency-associated malignancies. Dr. Swinnen is a member of the Eastern Cooperative Oncology Group and the National Comprehensive Cancer Network. Dr. Swinnen is rated as an Experienced provider by MediFind in the treatment of Immune Thrombocytopenic Purpura (ITP). His top areas of expertise are Non-Hodgkin Lymphoma, Diffuse Large B-Cell Lymphoma (DLBCL), Hodgkin Lymphoma, Small Lymphocytic Lymphoma (SLL), and Bone Marrow Transplant.
Rubenstein Child Health Building
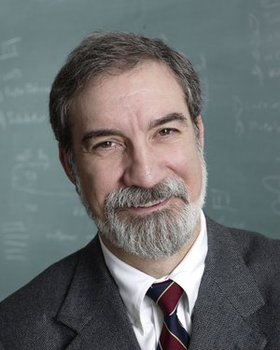
"Dr. James Casella is a professor of pediatrics and oncology at the Johns Hopkins University School of Medicine. As the Johns Hopkins’ Rainey Professor of Pediatric Hematology, Dr. Casella is chief of the Division of Pediatric Hematology at Johns Hopkins Children's and director of the Basic and Translational Research Program in Sickle Cell Disease, Comprehensive Sickle Cell Center and the Maryland Hemophilia Treatment Center at Johns Hopkins. He supervises several labs investigating the cellular and molecular basis of pediatric blood-borne diseases. He is seeking to develop better treatments for sickle cell disease and the prevention of central nervous system complications of this disorder, including stroke. Dr. Casella received his undergraduate degree in mathematics from Union College. He earned his M.D. from SUNY of Syracuse and completed a residency in pediatrics at Johns Hopkins University School of Medicine, where he was subsequently a fellow in hematology/oncology. He has been a member of the Johns Hopkins’ faculty since 1983. A research scientist as well as a clinician, he co-directs the hematology/oncology fellowship program at Johns Hopkins Hospital and is an adjunct senior investigator (Pediatric Oncology Branch) in the Division of Clinical Sciences, National Cancer Institute, National Institutes of Health. He is also director of the NHLBI-funded K12 in benign hematology program at Johns Hopkins that trains young clinician/investigators in benign hematology and transfusion medicine. Dr. Casella has served on numerous university, hospital, and advisory committees, many geared toward hematology, pediatrics and transfusion. He has received many awards from the Johns Hopkins Hospital, including the Alexander ""Buck"" Schaffer Award for Outstanding Contribution to the Teaching of House Officers. He and a colleague created the Johns Hopkins/St. Agnes Comprehensive Hemophilia Clinic to improve care for patients with the disease.". Dr. Casella is rated as an Experienced provider by MediFind in the treatment of Immune Thrombocytopenic Purpura (ITP). His top areas of expertise are Sickle Cell Disease, Congenital Hemolytic Anemia, Hemoglobinopathy, and Hemolytic Anemia.
Johns Hopkins Outpatient Center
Dr. Resar's studies molecular mechanisms leading to cancer, blood diseases, sickle cell anemia, hemophilia and other coagulopathies. Her research focuses on the HMG-I/Y gene family, which is widely overexpressed and functions as oncogenes in human cancers. Her laboratory recently developed transgenic mice overexpressing HMG-I; all mice develop aggressive lymphoid malignancy similar to leukemia and lymphoma in humans. Her studies also demonstrate that this gene is overexpressed in human lymphoid and other malignancies. Translational studies are underway to determine if overexpression of HMG-I is a marker for more aggressive human cancers. Resar's long-term goal is to develop more rational therapies that interfere with HMG-I/Y function in neoplastic transformation. Dr. Resar is rated as an Experienced provider by MediFind in the treatment of Immune Thrombocytopenic Purpura (ITP). Her top areas of expertise are Anemia, Sickle Cell Disease, and Immune Thrombocytopenic Purpura (ITP).
Rubenstein Child Health Building
Dr. Matthew Merguerian is a pediatric hematologist specializing in bleeding and clotting disorders. His research is focused on bleeding disorders resulting from platelet dysfunction. His lab is interested in understanding the mechanisms behind platelet dysfunction and in developing platelet-targeted therapies that could alleviate abnormal bleeding or clotting. Dr. Merguerian is rated as an Experienced provider by MediFind in the treatment of Immune Thrombocytopenic Purpura (ITP). His top areas of expertise are Blood Clots, Leukemia, and Immune Thrombocytopenic Purpura (ITP).
Johns Hopkins Children's Center
Dr. Kathryn Lemberg is an Assistant Professor of Oncology and Pediatrics at the Sidney Kimmel Comprehensive Cancer Center. Her research, conducted with Johns Hopkins Drug Discovery, focuses on tumor metabolism and the development of new metabolic inhibitors to treat cancer. She has investigated novel glutamine antagonists in preclinical models of RAS-driven solid tumors. She is also interested in the effects of tumor metabolism on patient growth and development. Dr. Lemberg completed pediatrics residency training at Johns Hopkins and pediatric hematology-oncology fellowship training in the joint Johns Hopkins/National Cancer Institute program. She received her M.D. and Ph.D. degrees from the Medical Scientist Training Program at Columbia University in New York, where her graduate research focused on ferroptosis, a novel oxidative cell death in cancer models. Dr. Lemberg sees pediatric and young adult sarcoma patients as part of the sarcoma team and has additional clinical focus on neurofibromatosis type I related solid tumors. . Her top areas of expertise are Malignant Peripheral Nerve Sheath Tumor, Neurofibromatosis Type 1 (NF1), Neurofibromatosis, and Adult Soft Tissue Sarcoma.
Johns Hopkins Children's Center
Dr. Friedman is the King Fahd Professor of Oncology and Professor of Pediatrics at the Johns Hopkins University School of Medicine and a member of the Johns Hopkins Kimmel Cancer Center. He received his M.D. from the Harvard Medical School (1983), did his pediatric internship and residency at Boston Children's Hospital (1983-86), and completed a fellowship in pediatric hematology-oncology at Johns Hopkins (1986-89). As a fellow, he did post-doctoral research at the Carnegie Institution Department of Embryology located on the Johns Hopkins Homewood campus. Dr. Friedman has served on the Pediatric Oncology faculty at Johns Hopkins since 1989. His laboratory focuses on investigation of normal and abnormal blood-cell formation. Dr. Friedman also cares for children with cancer, specializing in the treatment of leukemia. . His top areas of expertise are Leukemia, Glioma, Acute Lymphoblastic Leukemia (ALL), and Neuroblastoma.
Johns Hopkins Children's Center
Dr. Stacy Cooper is the Director of the Pediatric Hematologic Malignancy Program, Director of the Pediatric Hematology/Oncology Fellowship Program, and Clinical Director of the Pediatric Oncology Inpatient Program at the Johns Hopkins School of Medicine. Dr. Cooper received her undergraduate degree in Biology and Spanish at the University of Notre Dame. She earned her M.D. at SUNY Upstate Medical University. She completed her general pediatric residency and chief residency at the Johns Hopkins School of Medicine. She completed her pediatric hematology-oncology fellowship with the Johns Hopkins-National Institutes of Health. Dr. Cooper joined the Johns Hopkins faculty in 2015. Her research focuses on clinical research in acute lymphoblastic leukemia, as well as medical education scholarship related to fellowship training. Dr. Cooper is a member of the American Board of Pediatrics, the American Society of Hematology, the American Society of Pediatric Hematology Oncology and the Association of Pediatric Program Directors. . Her top areas of expertise are Classical Hodgkin Lymphoma, Hodgkin Lymphoma, Acute Lymphoblastic Leukemia (ALL), and Leukemia.
Johns Hopkins Children's Center
Robyn Gartrell, MD, MS is a physician-scientist and pediatric oncologist who joined the faculty at Johns Hopkins University School of Medicine as Assistant Professor in January 2024. Dr. Gartrell completed her clinical pediatric hematology/oncology fellowship at New York Presbyterian / Columbia University Irving Medical Center (CUIMC), and a postdoctoral fellowship in Immunotherapy and Precision Medicine. She also completed a Master of Science in Patient Oriented Research as well as her first 5 years as faculty at CUIMC. Dr. Gartrell’s primary research focuses on combination approaches including radiation, chemotherapy, and other target agents with immunotherapy to improve response, increase survival, and decrease toxicity for children, adolescents, and young adults with cancer. Her laboratory uses advances in tumor immunology to develop more effective and more personalized therapies using multiplex platforms and immunogenomics to evaluate the tumor microenvironment and determine which pediatric tumor types, and which patients, will respond to immunotherapy. . Her top areas of expertise are Glioma, Diffuse Midline Glioma H3 K27M-Mutant, HER2 Negative Breast Cancer, and Pancreatic Ductal Adenocarcinoma.
Rubenstein Child Health Building
Emily Rao is a Hematologist in Baltimore, Maryland. Her top areas of expertise are Sickle Cell Disease, Von Willebrand Disease (VWD), and Immune Thrombocytopenic Purpura (ITP).
Johns Hopkins Children's Center
Yiouli Ktena is a Pediatrics provider in Baltimore, Maryland. Her top areas of expertise are Graft Versus Host Disease (GvHD), Sickle Cell Disease, Immune Thrombocytopenic Purpura (ITP), and Bone Marrow Transplant.
Rubenstein Child Health Building
Recognized as a dedicated and compassionate pediatric hematologist-oncologist, Dr. Keates-Baleeiro cares for patients in the Division of Pediatric Hematology at Johns Hopkins Children’s Center in Baltimore, Maryland. A pediatric hematologist-oncologist is a physician who has special training and experience in diagnosing and treating blood disorders and cancers in children, teens, and young adults. Dr. Keates-Baleeiro’s current clinical interests include pediatric cytopenias, coagulation disorders, platelet disorders, sickle-cell anemia, and hemophilia. Her research interests include rare bleeding disorders, porphyria, and neutropenia in children. Dr. Keates-Baleeiro received her medical degree from the Drexel University College of Medicine in 1999 and completed her internship at Cohen Children’s Medical Center and her pediatric residency at Children’s Hospital of Michigan in Detroit in 2002. She then went on to complete a fellowship in pediatric hematology-oncology at the University of Michigan’s C.S. Mott Children’s Hospital and Vanderbilt University Medical Center in 2003 and 2006, respectively. Passionate about teaching, Dr. Keates-Baleeiro also serves as an Assistant Professor of Pediatrics at the Johns Hopkins School of Medicine educating medical students, pediatric residents, and pediatric hematology oncology fellows. . Her top areas of expertise are Phosphoglycerate Kinase Deficiency, Sickle Cell Disease, Hemoglobin SC Disease, and Infantile Neutropenia.
Johns Hopkins Children's Center
Yang Ding is a Pediatrics specialist and a Pediatric Hematologist Oncology provider in Baltimore, Maryland. Her top areas of expertise are Acute Lymphoblastic Leukemia (ALL), Leukemia, Neuroblastoma, and Langerhans Cell Histiocytosis.
Johns Hopkins Children's Center
Dr. Cohen is Director of Pediatric Neuro-Oncology and Clinical Director of the Division of Pediatric Oncology at the Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins. He received his undergraduate degree at Brown University and earned his MD at the Upstate Medical University, in Syracuse, NY. He did his general Pediatric Residency and Chief Residency at the University of Colorado and completed his Pediatric Hematology/Oncology Fellowship at Johns Hopkins. He has served on the faculty since 1994. His research centers on clinical trials of novel therapeutics for children with brain tumors. Dr. Cohen is co-chair of the High-Grade Glioma committee for the Children's Oncology Group and in that capacity has a particular research interest in the development of therapeutics for the treatment of infiltrating gliomas. He serves on the scientific advisory board for a number of organizations including St. Baldricks and the Childhood Brain Tumor Foundation. He is on the editorial board for PDQ with responsibility for authorship of the pediatric CNS brain tumor summaries. The Pediatric Neuro-Oncology program conducts a broad range of research centered primarily around the development and testing of novel therapeutics for children with brain tumors. The multidisciplinary nature of this work translates into continual collaboration with specialists in pediatric neurosurgery, radiation oncology, neuropathology, neuroradiology, neurology, neuro-ophthalmology, neuropsychology, and other related disciplines. . His top areas of expertise are Glioma, Brain Stem Cancer, Medulloblastoma, Embryonal Tumor with Multilayered Rosettes, and Bone Marrow Aspiration.
Johns Hopkins Children's Center
Dr. Koldobskiy is an Assistant Professor of Pediatric Oncology and Pediatric Neuro-Oncology at the Sidney Kimmel Comprehensive Cancer Center. He received his B.S. and M.S. from Yale University and M.D./Ph.D. in the Medical Scientist Training Program at Johns Hopkins, conducting his thesis research with Dr. Solomon Snyder in Pharmacology and Molecular Sciences. He completed his Pediatrics residency training at Johns Hopkins and his Pediatric Hematology and Oncology fellowship training in the joint Johns Hopkins/National Institutes of Health program. He studies epigenetic variability in childhood cancer. . His top areas of expertise are Leukemia, Glioma, Teratoma of the Mediastinum, and Acute Lymphoblastic Leukemia (ALL).
Johns Hopkins Children's Center
Dr. Bonifant is a pediatric oncologist on the blood and marrow transplantation team at the Sidney Kimmel Comprehensive Cancer Center and an Assistant Professor of Pediatric Oncology at the Johns Hopkins University School of Medicine. She is also a member of the Bloomberg-Kimmel Institute for Immunotherapy. Her clinical specialty is stem cell transplantation for high-risk leukemias. Her research interests are in the areas of immunotherapy of cancer and malignant hematology. Currently, her research focuses on design and development of immune therapies as a treatment for poor-prognosis cancers, including development of engineered cellular immunotherapies for the treatment of Acute Myeloid Leukemia. Dr. Bonifant is a graduate of Wake Forest University and Georgetown University. She completed her Pediatric and Hematology/Oncology training at Johns Hopkins and at Baylor College of Medicine. Prior to her appointment at Johns Hopkins, she was an Assistant Professor in Pediatrics-Hematology/Oncology at the University of Michigan. . Her top areas of expertise are Leukemia, Infantile Neutropenia, Acute Lymphoblastic Leukemia (ALL), and Childhood Acute Myeloid Leukemia.
Johns Hopkins Children's Center
Dr. Cooke is Director of the Johns Hopkins Kimmel Cancer Center’s Pediatric Bone Marrow Transplantation Program. Prior to his appointment at Johns Hopkins, Dr. Cooke headed the Pediatric Blood and Marrow Transplantation Program at Rainbow Babies and Children’s Hospital, and University Hospitals Case Medical Center, in Cleveland, Ohio. He also co-directed the Hematologic Disorders Program of the Case Comprehensive Cancer Center at Case Western Reserve University. A nationally recognized transplantation immunology expert, Dr. Cooke focuses primarily on new strategies to prevent and treat graft-vs-host disease and lung complications following blood and bone marrow transplantation. His research efforts have been recognized by the Leukemia and Lymphoma Society and the American Society of Clinical Investigation. In addition to his younger patients, Dr. Cooke also cares for adolescents and young adults. . His top areas of expertise are Graft Versus Host Disease (GvHD), Chronic Graft Versus Host Disease (cGvHD), Anemia, Aplastic Anemia, and Bone Marrow Transplant.
Johns Hopkins Children's Center
As instructor of oncology and pediatrics, Llosa’s research focus is the immunotherapy of sarcomas. My research focuses on understanding how the immune system interacts with cancer cells from sarcoma tumors. Sarcoma is a type of cancer that can occur in various locations in the body. Sarcoma is the general term for a broad group of cancers that includes tumors that form in the bones and in the soft (also called connective) tissues. Sarcomas affect people of all ages and some, such as Rhabdomyosarcoma, Neuroblastoma, Ewings sarcoma and Osteosarcoma, are more common in children and young adults. Treatments for sarcoma vary depending on tumor type, location and other factors. I concentrate in the immunotherapy of sarcomas. Immunotherapy (also called biologic therapy or biotherapy) is a type of cancer treatment designed to boost the body's natural defenses to fight the cancer. It uses materials either made by the body or in a laboratory to improve, target, or restore immune system function. Immunotherapy works by stopping or slowing the growth of cancer cells, stopping cancer from spreading to other parts of the body, or helping the immune system increase its effectiveness at eliminating cancer cells. There are several types of immunotherapy, including monoclonal antibodies, non-specific immunotherapies, and cancer vaccines. My specific area of interest is the use of drugs that target immune system checkpoints. The immune system has checkpoints to keep itself from attacking other normal cells in the body. Cancer cells sometimes take advantage of these checkpoints to avoid being attacked by the immune system. CTLA-4 and PD-1/PD-L1 are checkpoint molecules found on immune system cells (T cells) that can be blocked with drugs leading to a general raise in the immune system of the patients which helps it attack cancer cells. These types of drugs are currently being given to patients with melanoma (skin cancer), lung cancer and kidney cancer with great success and they have been found to shrink advanced tumors in many people. The best part of the treatment is that many of these tumor responses have been long-lasting so far, and the side effects are generally less serious than when using chemotherapy. Larger clinical trials are now studying both drugs, both alone and/or in combination with other treatments. My task is and will continue to be using the same type of approach for attacking sarcomas and hopefully obtained the very promising results and long lasting responses observed with the use of immune checkpoint inhibitors in other types of cancer. . His top areas of expertise are Adult Soft Tissue Sarcoma, Osteosarcoma, Malignant Peripheral Nerve Sheath Tumor, Ewing Sarcoma, and Bone Marrow Transplant.
Last Updated: 01/09/2026